Translate this page into:
The Middle Mesial Canal: Combined Endodontic and Restorative Treatment Approach - A Case Report

*Corresponding author: Dr. Abeer Babiker Hamad El Nil, Department of Restorative Dentistry, Private Practice, Dubai, United Arab Emirates. abeer.babiker@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Nil ABH. The Middle Mesial Canal: Combined Endodontic and Restorative Treatment Approach - A Case Report. Dent J Indira Gandhi Int Med Sci. 2024;3:115-120. doi: 10.25259/DJIGIMS_19_2024
Abstract
The management of the middle mesial canal (MMC) in mandibular first molars presents considerable challenges during endodontic treatment due to its complex anatomy. Challenges may arise throughout various stages of treatment, including canal location, instrumentation, and obturation. The inability to identify and shape this canal can lead to endodontic failure and post-treatment apical periodontitis. Therefore, understanding this aberrant root canal anatomy and its clinical implications during the various stages of endodontic treatment is essential for successful management, including the selection of the optimal coronal restoration to enhance the efficacy of the obturation’s coronal seal and to ensure the restoration’s maximal longevity. This case report describes the diagnosis and successful endodontic and restorative management of an MMC in a mandibular first molar.
Keywords
Middle-mesial-canal
Mandibular-molar
Irreversible-pulpitis
Mesial-canals
Composite-onlay
INTRODUCTION
The mesial root of the mandibular first molar generally has two canals, the mesiobuccal (MB) and mesiolingual (ML) canals, while the distal root often has one canal.[1] Complex anatomy is frequently observed in the mesial root, with the MMC having a general incidence of 46.2%.[2] Incidences of MMCs have also been reported in various races, including 53.8% in some populations.[3] MMCs have been reported in Asians, Europeans, South and North Americans, and Africans.[3]
Versiani and Nosrat noted differences in the incidence of MMCs between the Brazilian and Turkish populations, as well as between White (12.2%) and non-White (29.4%) races.[3] In India, Shriya and Anuja reported a low prevalence of 5.7% in mandibular molars in the Vidarbha region of central India’s population in their cross-sectional study.[4] Conversely, Sana and Iqbal reported a higher prevalence of 21.8% in mandibular first molars in the Greater Noida region of northern India in their retrospective study.[2]
The incidence is generally higher in younger patients: 32.1% in those aged ≤20 years, 23.8% in those aged 21–40 years, and 3.8% in those over 40 years.[3] Few studies have reported significant differences in the prevalence of MMC between genders or in unilateral or bilateral incidence.[1] Nosrat and Pomeranz reported an equal incidence in both mandibular molars.[3] However, most studies have reported a higher incidence in the first mandibular molars, with only a few studies reporting a higher incidence in the second mandibular molars.[4]
Barker, Vertucci, and Williams were the primary researchers to discover the presence of an extra independent canal in the mesial root of mandibular molars known as the MMC.[2] Pomeranz then classified it into three types: independent, confluent, and fin.[5] The fin type occurs when an instrument passes freely within the MB, ML, or MMC canal.[5] The confluent type is when the MMC starts as a distinct orifice but merges apically with the MB or ML canal, while the independent type is when the MMC starts as a separate orifice and ends with a separate foramen.[5] A large single mesial canal where three master cones may be cemented to the apex is considered an independent MMC.[2]
Azim reported a high incidence of confluent type (78.5%), followed by fin-type (12%) and independent type (9.5%).[1] Nosrat reported that 46.7% of the MMC were confluent type, 33.3% were fin type, and 20% of the canals were independent type.[4] Additionally, 42% of the MMC merged with the (MB canal, while 29% merged with the ML canal.[4]
Challenges in managing MMCs are often encountered during the three stages of endodontic treatment:
-
1.
-
2.
-
3.
Obturation: The mean minor diameter of the MMC orifice is approximately 0.16 mm, which is three times smaller than the diameter of the two main orifices (0.50 mm), creating difficulty in master-cone insertion and compaction.[1]
Therefore, the objective of this case report is to highlight the common challenges encountered during the endodontic treatment of MMCs and to provide insights into the successful endodontic restorative management of a Mesiolingual-confluent case variant of the MMC in mandibular first molars, which is less frequently reported in the literature.
Case Report
A 17-year-old male presented with spontaneous, throbbing pain on tooth 36 for the past 5 days. Clinical examination revealed a fractured composite restoration with pain on probing, which was further exacerbated by the application of endo-ice-refrigerant spray (Coltene Whaledent, Altstatten, Switzerland) [Figure 1a-b]. The tooth was tender to percussion but negative to palpation, with normal probing depths on periodontal examination. Radiographic examination showed a large restoration close to the mesial pulp horn and a widening of the periodontal ligament on both roots [Figure 1c-d]. Consequently, a diagnosis of symptomatic irreversible pulpitis with symptomatic-apical periodontitis was made.

- Tooth no. 36 with fractured composite restoration buccally. Buccal view.

- Tooth no. 36 with fractured composite restoration buccally. Occlusal view.

- Pre-operative periapical radiograph showing large restoration (composite) close to the mesial pulp horn in 36.

- Periapical pre-operative radiograph showing widening of the periodontal ligament on both root of 36.
1. Endodontic treatment:
Following the patient’s informed consent, an inferior alveolar nerve block was administered using 1.8ml of lidocaine HCl 2% with epinephrine 1:80000. A rubber dam was placed, and the restoration was removed using high-speed round bur. Access cavity preparation was refined using an Endo-Z-bur (Dentsply Sirona, North Carolina, USA). The pulp chamber was explored using a DG-16 explorer, and the canals were initially negotiated with size 8k files (DiaDent, Burnaby, Canada). Three canals were initially located: two mesial and one distal canal. A groove, lighter in color compared to adjacent dentin, was found under a dentinal projection on the mesial axial wall, equidistant from the MB and ML canals, with a bleeding point at its center. Using magnification with a dental loupe and light-emitting diode (3.5×, 420 Dentrics, China), the MMC was located with an endodontic explorer and carefully negotiated with a size 8K file. Troughing was performed with ultrasonic tips ET18D (Aceton Endosuccess, Ontario, Canada).
A total of four distinct orifices were identified: three mesial (MB), middle mesial, ML, and one distal [Figure 2a]. The working length was determined using an apelocator or (Ruby Endo Art, London) and periapical radiographs taken at various angles. The working-length radiograph revealed that the MMC was of a confluent type, emerging as a separate orifice and joining the ML canal from midfoot to apex [Figure 2b]. The canals were shaped and cleaned in a crown-down manner using the ProTaper Universal rotary system (Dentsply Maillefer, North Carolina, USA), finished with F1 for all mesial canals due to their narrow diameter and F2 for the distal canal [Figure 2c]. A 3% warm sodium hypochlorite solution was used for irrigation with a side-vented needle. EDTA gel (17%) (Canal+, Septodent, Saint-Maur-des-Fosses, France) was used as the final rinse for smear-layer removal, followed by saline. The canals were dried using paper points. Obturation was completed using initially cold lateral compaction of Gutta-percha cones in the canal’s apical third, followed by warm vertical compaction technique using (6% taper Gutta-percha cones), resin sealer (AH Plus Sealer, Dentsply Sirona, USA), and an EQ-V plus gun (Meta-Biomed, Chungcheongbuk-do, Korea) [Figure 3a].
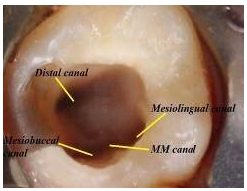
- Access cavity showing the location of the middle mesial canal in the center of the groove, between the mesiobuccal and distobuccal canal.
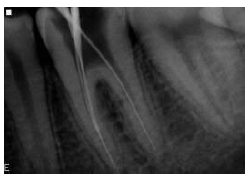
- Working length radiograph showing confluence of the middle mesial canal (MMC) with the mesiolingual canal.
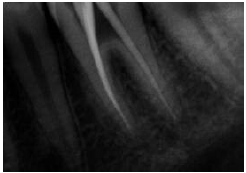
- Master cone radiograph showing confluence of the middle mesial canal (MMC) with the mesiolingual canal.

- Access cavity after obturation of the canals.
Glass ionomer cement was placed on the cavity floor to seal the canal orifices, followed by flowable composite as a base [Figure 3b]. Cavit (3M ESPE, Bayern, Germany) was used as a temporary restoration for 2-weeks due to its composite-like properties, which provide superior mechanical strength compared to conventional zinc oxide-eugenol temporary fillings. With its low polymerization shrinkage and solubility, Cavit is suitable for indirect onlay cavity preparations or (cuspal replacement restorations) subjected to strong occlusal forces.

- Access cavity after sealing the canal orifices with glass-ionomer-cement, followed by the placement of flowable composite, as a base for the indirect composite onlay and cavity preparation.
2. Restorative-treatment:
After 2 weeks, the temporary filling was removed, and cavity undercuts were blocked with flowable composite. The buccal wall and Bucco-occlusal cavity walls were prepared and reduced by 1 mm with a chamfer bur to increase their divergence. The internal and external cavity linings were rounded to a 90-degree cavosurface margin. A 1-mm deep chamfer margin was prepared on the buccal cervical wall for the composite onlay. Next, the cavity was cleansed and dried. Shade selection and a dual-phase impression technique were used (Waldent FlexiDent, Delhi, India), and the impression was sent to the laboratory.
At the next visit, the restoration fitting was verified, and the laboratory-sandblasted silanated composite onlay was cemented according to the manufacturer’s instructions (Ivoclar Variolink, Zurich, Switzerland). The restoration was then finished, polished, and occlusal high points were removed [Figure 3c-4a].

- After composite onlay cementation.
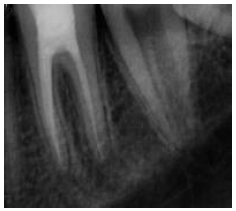
- Immediate post-treatment periapical obturation radiograph, showing confluence of the middle mesial canal with the mesio-lingual canal and after cementation of the indirect composite onlay.
DISCUSSION
Many studies in the literature have demonstrated that the MMC orifice is closer to the ML canal than to the MB canal, with some studies reporting an equidistant location from both canals.[1] Sherwani concluded that in 67% of the North Indian population, the orifices of MMCs were equidistant from MB and ML canals.[4] In 20.5% of cases, the orifice was closer to the ML canal, and in 12.3% of cases, it was closer to the MB canal.[4] The average distance between the MB and ML canal is approximately 3.1 mm in molars with MMCs and 3.7 mm in molars without MMC.[1] MMCs are identified more frequently in mandibular first molars with an isthmus between the MB and ML canals.[3] Their mean diameter and volume are 2–3 times smaller than those of the main canals.[1] Most MMCs exhibit moderate to severe curvature starting from the midroot, with prominence in either the mesiodistal or buccolingual direction, and this curvature tends to decrease with age due to calcification.[1]
MMCs are frequently found in young adults with complete-isthmus connecting the two major canals and in mandibular first molars having two distal canals (45.4 %) more often than those with one distal canal.[1] The confluent type, where the MMC merges with the MB canal, is often observed.[3] However, in this case, the MMC was found equidistant from both the MB and ML canals, in agreement with Sherwani’s study, and it confluences with the ML canal. Only one distal canal was found, which aligns with Nosrat’s findings that reported no correlation between MMCs and the presence of a second distal canal.[3]
Failure to understand MMC anatomy can subsequently lead to endodontic treatment failure and post-treatment apical periodontitis.[5] Mashyakhy found that the frequency of post-treatment apical periodontitis in endodontically treated teeth with missed canals was 90%. Karabucak and Baruwa reported slightly lower percentages at 82.8% and 82.6%, respectively.[6]
Challenges in access cavity preparation often arise as a result of failure to remove dentinal protuberance from the mesial-axial wall or from using a conventional handpiece, which can prevent direct visualization and access to the developmental dentinal groove between the MB and ML orifices. This groove is lighter in color compared to the surrounding dentin and should be carefully examined with an endodontic explorer.[1] If depression or orifices are located, the groove may be troughed with ultrasonic tips at its mesial aspect until a small file can negotiate the MMC (guided troughing technique).[1]
Various diagnostic aids, such as champagne bubble tests, dye tests, ultrasonics, micro-openers, and transillumination, improve pulp chamber visibility.[1] Observing for bleeding points in orifices, grooves, and isthmuses (red line test) provides a roadmap for finding additional canal orifices.[1] Moreover, the use of magnification aids, such as magnifying loupes or dental microscopes, and the use of multiple angulated radiographs or cone-beam computed tomography (CBCT) are advised to limit procedural errors during canal exploration.[5] However, CBCT should be used only when additional details are required for diagnosis and treatment planning due to their high ionizing radiation and cost.[5]
During instrumentation, procedural errors often occur due to the narrow, curved, or joined nature of MMCs.[1] The crown-down instrumentation technique is preferred, and small or intermediate-size (12-17) rigid-K- files with high buckling-resistance or C+ files may be used, as they can efficiently negotiate and progress through the narrow canal without bending, using a watch-winding-motion and being continuously flooded with sodium hypochlorite.[1] A cautious brushing motion should be employed away from the furcation and towards the root’s mesial side.[1] The apical enlargement and obturation should consider the minor diameter of the apical constriction configuration.[1] Preparing them to smaller sizes with a small taper, preferably 4%, is desirable.[1] Different obturation techniques may be employed depending on the root canal configuration.[1] However, cold lateral compaction/condensation of Gutta-percha in the apical third, with or without vertical compaction of the remaining MMC canal using thermoplasticized gutta-percha, is a common obturation technique,[1] which was also used in this case report, following the above biomechanical-preparation guidelines.
From a restorative perspective, ceramic onlays have traditionally been preferred over composites for cuspal replacement in endodontically treated teeth due to their superior compressive strength, wear resistance, and aesthetics. Direct composites often face such as marginal leakage, fracture, high wear rates, post-operative sensitivity, and secondary caries, attributed to high polymerization-related issues.[7] However, these poor mechanical properties were significantly improved later with the introduction of micro-hybrid or nanofillers, external light curing, and glass fiber reinforcement.[7]
Bondable ceramics mimic enamel’s flexural strength and fracture toughness.[7] Composites match the elastic modulus of dentin, which helps in transferring decreased masticatory forces compared to ceramics, which are weaker under shear forces and may abrade the opposing teeth.[8] Conversely, composites have a greater capacity to absorb compressive loading, reducing impact forces by 57%, and do not abrade the opposing teeth.[7]
Tooth vitality can variably influence the clinical performance of both materials.[9,10] In two in vitro studies by Magne, which tested the influence of load cusps and mechanical loads on the fatigue resistance of endodontically treated teeth, composite onlays had higher fatigue resistance and a lower fracture rate compared to ceramics.[9,10] Therefore, considering the above factors and the conservative nature of the composite’s onlay, it was considered the appropriate restoration for this young patient. After 2-years of follow-up, there was excellent healing of the periapical tissues, with the coronal restoration remaining intact [Figure 4b].

- Post-obturation periapical radiograph after 2-year’s follow-up showing healing of the periodontal tissues and intact coronal restoration.
CONCLUSION
The variable location and narrow, curved configuration of the MMC make canal identification, preparation, and obturation very challenging. Understanding the complex anatomy of the MMC is the key to successful endodontic treatment and is supplemented by the use of various diagnostic aids, advanced radiographic imaging modalities, magnification, accurate instrumentation, and cautious obturation. With regards to the restorative aspect of the case, the indirect composite onlay proved to be a successful, viable option for restoring endodontically treated teeth, as confirmed by the 2-year follow-up and in agreement with the above-mentioned studies.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of Artificial Intelligence (AI)-Assisted Technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
REFERENCES
- Middle mesial canal in mandibular first molar: A narrative review. Saudi Dent J. 2023;35:468-75.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Prevalence of middle mesial canal in the Indian subpopulation of Greater Noida and the related variations in the canal anatomy of mandibular molars using cone-beam computed tomography. Endodontology. 2022;34:50-4.
- [CrossRef] [Google Scholar]
- Middle mesial canals in mandibular molars: Incidence and related factors. J Endod. 2015;41:28-32.
- [CrossRef] [PubMed] [Google Scholar]
- Frequency of middle mesial canals in mandibular first molars in North Indian population - An in vivo study. Saudi Endodontic J. 2016;6:66-70.
- [CrossRef] [Google Scholar]
- Unveiling hidden canals: Middle mesial canal prevalence in mandibular first molars using cone-beam computed tomography analysis in central India. Cureus. 2023;15:e45944.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Prevalence of missed canals and their association with apical periodontitis in posterior endodontically treated teeth: A CBCT study. Int J Dent. 2021;2021:9962429.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Indirect resin composites. J Conserv Dent. 2010;13:184-94.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Composite versus Ceramic for large posterior restoration. J Inside dentistry. 2022;18:8.
- [Google Scholar]
- Influence of overlay restorative materials and load cusps on the fatigue resistance of endodontically treated molars. Quintessence Int. 2009;40:729-37.
- [PubMed] [Google Scholar]
- Porcelain versus composite inlays/onlays: Effects of mechanical loads on stress distribution, adhesion, and crown flexure. Int J Periodontics Restorative Dent. 2003;23:543-55.
- [PubMed] [Google Scholar]







