Translate this page into:
RADICULAR CYST : A CASE SERIES WITH REVIEW OF LITERATURE
Corresponding Author : Dr. Abhay Kulkarni
This article was originally published by Indira Gandhi Institute of Medical Science and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Radicular cysts are the most common odontogenic cystic lesions of jaws, these are inflammatory in origin. These cysts result from the proliferation of cell rests of Malassez in the periodontal ligament as a consequence of inflammation, following pulpal necrosis of a nonvital tooth. The condition is usually asymptomatic but can result in a slow-growth in the affected region. On radiography the lesion is often seen as a round or oval, well circumscribed radiolucent area involving the apex of the infected tooth. Nonsurgical management should be the treatment of choice of a radicular cyst. However, periapical surgery is often considered, if the lesion is extensive and fails to reply to a nonsurgical approach.
The case report is of a 43-year-old male patient with the complaint of swelling in an anterior region of maxilla since past 2 months which was gradually increase in size with no history of any pain or pus discharge. Patient had history of root canal treatment with upper right canine 10 years back.
The second case report is of 45-year-old male patient with the complaint of pus discharge from destructed teeth in anterior region since one month. No intraoral and extra oral swelling present.
The third case report is of 15 yrs. old male patient with the complaint of pain in upper anterior tooth since 7 days. Patient had history of root canal treatment with right lateral incisor 2 months back.
The definitive diagnosis was made based on clinical, radiological and histopathological examination. Both the case reports discusses detailed description of clinical, radiographic, histopathologic features, pathogenesis, and its surgical management.
Keywords
Bay cyst
Radicular Cyst
Nonvital tooth.
INTRODUCTION:
A cyst is defined as a pathological cavity having fluid, semi fluid, or gaseous contents, which is not created by accumulation of pus (Kramer, 1974).1 Cysts are classified into odontogenic and nonodontogenic based on the tissue they arise from. Odontogenic cysts are often broadly divided into developmental and inflammatory cyst based on their aetiology. Radicular cyst and lateral periodontal cyst are classified as inflammatory odontogenic cysts. The most common inflammatory odontogenic cysts in tooth bearing areas of the jaws are radicular cysts (apical periodontal cyst, dental root end cyst).2 They originate from an epithelial rest of Malassez in periodontal ligaments secondary to inflammation.3 They are most often found at the apices of the involved teeth with infected or necrotic pulps; however, they will even be found on the lateral aspects of the roots in relation to accessory root canals.4
Radicular cyst is mostly seen during the third and fifth decades of life, and common in males.5 clinically radicular cysts are symptomless and are noted when radiographs are taken of non-vital teeth. Patient complains of slowly enlarging swelling.6 Radiographically most radicular cysts appear as round or pear-shaped unilocular radiolucent lesions within the periapical region. The cysts may cause root resorption or displacement of adjacent teeth.6
Histopathologically, the radicular cyst is a chronic inflammatory lesion with a closed pathological cavity. It is lined by non-keratinised stratified squamous epithelium.3 Radicular cysts must be totally enucleated surgically to remove all epithelial remnants. Endodontic treatment or extraction leads to spontaneous healing of radicular cyst.7
The present case series documents with the cases of radicular cyst in anterior maxilla along with its histopathology and surgical management.
CASE REPORT: 1
A 43-year-old male patient with the complaint of small sized gradually growing swelling in an anterior region of maxilla since the past 4 months. The swelling was not associated with any pain or pus discharge. The patient does not recall any history of trauma. Patient had history of RCT with right upper canine 10 years back and apical puff was achieved, which was confirmed radiographically. His past medical history was non-contributory.
Extraoral examination revealed no facial swelling or obvious facial asymmetry. On intraoral examination, (fig. A & B) there were restorative filling with teeth 12. Inspectory findings revealed an asymptomatic diffuse buccal swelling on the right side, which was extending from 11 anteriorly to 14 posteriorly. The swelling measured about 2 cm × 1.5 cm in its largest dimension. No evidence of any surface changes / bleeding / sinus opening / pus discharge. On palpation, the swelling was non-tender, ovoid in shape, soft in consistency, non-fluctuant, and nonpulsatile with no mobility of the involved teeth. The overlying palatal mucosa appeared normal.

- Intraoral swelling on buccal sulcus

- Normal palatal mucosa
The patient was advised for routine cone beam computed tomography for right maxilla for radiological evaluation, which revealed that buccal and lingual cortical plate were intact. (Fig. C) There was a homogenous radiopacity in 12 region. A well- defined radiolucent lesion noted at periapical region with 12. It extends from mesial aspect of 13 tooth root till mesial aspect of 21 tooth root region size approximately 1.25 cm × 1cm. Expansion of lingual and buccal cortical plates were noted. Periphery of shape of lesion shows well defined smooth and corticated borders on radiograph. There was no evidence of root resorption/displacement of the adjacent Teeth. The radiographic findings were suggestive of radicular cyst.

- cone beam computed tomography for right maxilla
CBCT was considered as imaging modality choice as the clinical, radiographic, histological diagnosis of periapical lesions has been a challenge, and differentiating between the varied periapical lesions remains an open research problem. Attempt to diagnose, the lesion before surgery with intraoral periapical (IOPA) radiographs, contrast media, Papanicolaou smears, and albumin tests have proven to be inaccurate. Thus, there is a requirement for a non-invasive method to diagnose lesions involving the periapical area. Recently with the arrival of imaging modalities like CBCT.
The patient was advised for surgical excision under local anaesthesia after obtaining an informed consent from the patient. Crevicular incision was made from 21 to 14 with Vertical releasing incision and the trapezoidal mucoperiosteal flap was raised. The overlying thinned bone was removed with bur under copious irrigation to expose the cystic mass. Careful enucleation of cyst was performed along with apicectomy of root canal treated tooth 12 and curettage was done. (Fig. D) Flaps were repositioned and sutures were taken with 3-0 vicryl. (Fig. F) Excised tissue was sent for histopathological investigation. (Fig. E) Necessary prescriptions and postoperative instructions were given.

- Enucleation with Apicectomy

- Excised Lesion

- Sutures placed
Differential diagnosis includes dentigerous cyst, pindborg tumour, periapical cementoma, traumatic bone cyst, ameloblastoma, odontogenic keratocyst and odontogenic fibroma. Confirmatory final diagnosis of the radicular cyst is established only after surgical biopsy and histopathological examination of the lesion.
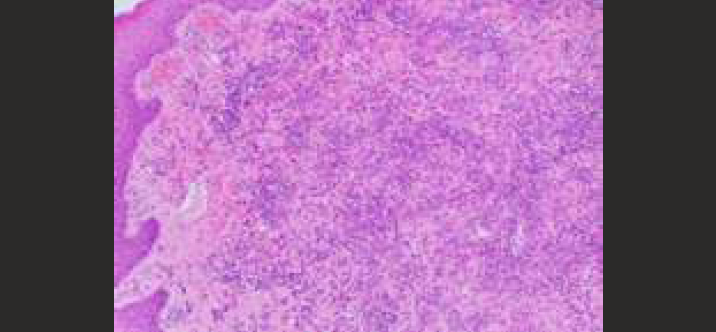
Histopathological examination revealed a cystic cavity lined by nonkeratinized stratified squamous epithelium arranged in an arcading pattern, interspersed with intense inflammatory cell infiltration consisting chiefly of lymphocytes and plasma cells. Russel's bodies were also noted at places. The histopathological findings confirmed the diagnosis of radicular cyst. (Fig. G) Based on clinical radiographic and histopathological findings the provisional diagnosis radicular cysts with 12 was made.
- Photomicograph
CASE REPORT 2:
A 45-year-old male patient reported with the chief complaint of pus discharge from destructed teeth in the upper front region of the jaw since 1 month. He had a history of grossly carious teeth in upper anterior region since 12 years.
The clinical examination revealed grossly carious teeth with 11 and Pus discharge was seen from the canal with 11 and 21. No intraoral swelling was noted. The teeth were tender on percussion. Buccal vestibule of upper anterior region was painful on palpation. Teeth 11 and 21 had grade 1 mobility (fig. H).

- Intraoral Image
Patient was advised for an OPG. Radiographic examination revealed a nonhomogeneous large radiolucency involving 11, 12, 21, and 22 with ill- defined radiopaque corticated borders. An external root resorption was seen along with displacement in relation to 11 and 21 suggestive of infected radicular cyst (fig. I).

- OPG
After obtaining an informed consent from the patient; he was advised for surgical excision under local anaesthesia. After giving the local anaesthesia all the four teeth that is 11, 12, 21, 22 were extracted and then the mucoperiosteal flap was raised. To expose the cystic mass the overlying thinned bone was removed with bur under copious irrigation. Careful enucleation of cyst was performed (Fig. J). Flaps were repositioned and sutures were taken with 3-0 vicryl (Fig. K). Necessary prescriptions and postoperative instructions were given and patient was recalled after 10 days (Fig. L).

- Surgical enucletion and excised lesion along with extracted teeth

- Sutures placed

- After suture removal
CASE REPORT 3:
A 15 Yrs old male patient came with the chief complaint of pain in right upper tooth since 7 days. He had given history of pain since 7 days, which was mild, dull aching, aggravated on chewing food, relieved on taking painkiller. Past dental history revealed root canal treatment with right lateral incisor. Clinical examination revealed mild expansion of buccal cortical plate in relation to 12. Teeth were tender on percussion. Vestibular tenderness in the region of 12 and 11 was noted. On radiographic examination, Radiopacity was noted in pulp canal of 12 suggestive of root canal filling material. A well-defined radiolucency with corticated margin in relation to apical region of 12 suggestive of radicular cyst. (Fig M) The patient was advised for surgical excision under local anaesthesia after obtaining an informed consent from the patient. After giving the local anaesthesia, the mucoperiosteal flap was raised. Careful enucleation of cyst was performed (Fig N). Flaps were repositioned and sutures were taken with 3-0 vicryl (Fig. O) Necessary prescriptions and postoperative instructions were given and patient was recalled after 10 days.

- IOPA of 12 region

- Surgical enucleation

- Sutures placed
DISCUSSION:
Periapical cysts are inflammatory jaw cysts that appear at the apices of infected teeth with necrotic pulps. Periapical cysts were classified as bay cysts or apical cysts based on the opening or connection of the root canal to the epithelium walled cavity. Bay cyst, which is now termed as "periapical pocket cysts” due to its similarities with the marginal periodontal pocket is the cystic cavity with epithelial linings that are open to the root canal whereas a cystic cavity with complete epithelialization but no opening into the apical foramen and root canal is considered as apical cyst.8 At present, it is mentioned as radicular cyst/true cyst. Study done by Ricucci D et al had suggested that except for morphologic relationship of the cyst cavity with root canal space, true and bay cysts exhibited no other significant differences.9 These findings are concurrent with our study. Sometimes, the cyst may appear on the lateral aspect of the root when the lesion is related to lateral accessory root canals. Among all the jaw cysts, radicular cysts count about 52%-68%.10
Prevalence of the radicular cysts within the maxilla is 60% as compared with mandible, and is related with buccal or palatal enlargement. The present cases was associated with a buccal swelling.
With a range of 0.5 percent to 3.3 percent, it affects both the primary and permanent dentition. They are more common in males compared to females with a ratio of 1.6:1. Females are more conscious about their teeth, which could explain why females have a lower incidence of the lesion.8
The anterior maxilla is more common as compared to the mandible. The involvement of anterior maxilla could also be due to trauma, caries, and old silicate restorations within the anterior teeth. In this case, there is no history, which was contributory. There are various opinions suggests for explaining the formation of this cyst. The pathogenesis of radicular cyst was described by Torabinejad (1983) in terms of "breakdown/nutritional deficit hypothesis" and "abscess cavity theory." However, the foremost accepted theory is that the epithelial breakdown theory as also supported by previous articles.8,11
Radicular cystic lesions undergo asymptomatic evolution with crepitations followed by erosion and fluctuation of the overlying soft tissue. The bone within the surrounding area will be thinned out with springiness and egg shell crackling, resulting in cortical plate expansion. The alveolar ridge exhibits a paper-like texture on palpation.12
Radiographically, the radicular cyst appears as round or pear-shaped unilocular radiolucency at the apex of a non-vital tooth. A radicular cyst's margin is radiopaque, with hyperostotic borders which continues with the lamina dura.. However, in infected or rapidly enlarging cysts, the radiopaque margin might not be present. The resorption of offending tooth roots may occur as a result of a chronic radicular cyst. In our case there is no root resorption. Other odontogenic cysts like dentigerous cysts, odontogenic keratocysts and odontogenic tumours like ameloblastoma, Pindborg tumour, odontogenic fibroma and cementoma may share and equivalent radiological features as radicular cysts. Hence histopathological evaluation is important most of the time to diagnose these sorts of giant lesions. In extensive cases, radiographs alone might not be sufficient to point out the complete extent of the lesions, and advanced imaging could also be needed. Hence, in this case we advise CBCT to the patient.
Histopathologically, radicular cysts are lined completely or partially by stratified squamous epithelium. These linings could also be discontinuous partially and range in thickness from 1 to 50 cell layers. A cyst's lumen contains a low-protein fluid and a collection of cholesterol clefts (Rushton bodies) with multinucleated giant cells. Acute and chronic inflammatory infiltrates of various intensities are present subepithelially. Few cases are reported with hyaline bodies which represent a secretory product of the odontogenic epithelium in radicular cyst. The disintegration of red blood cells, lymphocytes, plasma cells, and macrophages results in the formation of cholesterol crystals. In this case, histopathological examination revealed a cystic cavity lined by nonkeratinized stratified squamous epithelium arranged in an arcading pattern, interspersed with intense inflammatory cell infiltration consisting chiefly of lymphocytes and plasma cells. Russel's bodies were also noted at places.12
The treatment of the radicular cyst depends on the dimensions and localization of the lesion. Endodontic therapy, extraction, surgical procedures such as enucleation, and marsupialization are all alternatives for its treatment.5 In our first case, the treatment of choice was surgical enucleation and curettage along with apicectomy of root canal treated tooth 12. In our second case, the treatment of choice was surgical enucleation along with extraction of 11, 12, 21, 22. In third case, the treatment of choice was surgical enucleation.
A few well-documented cases indicate that squamous carcinoma occasionally arises from the metaplastic changes within the epithelial lining of the radicular cysts. Histopathological evidence of transition from a cystic lining to epithelial dysplasia and further progression as infiltrating squamous cell carcinoma has been seen in long-standing cases of radicular cysts.13 One report in the literature describes the formation of squamous odontogenic tumor like proliferations within the lining of radicular cysts. Around 3.5% of the time, these situations occur. The most prevalent site for such change was a radicular cyst in the maxillary area.14 Therefore, the treatment of radicular cysts should be prompt to avoid any potential complications and clinicians should remember of the remote chances of radicular cyst converting into squamous carcinoma.
If untreated, the radicular cyst slowly increases in size at the expense of the surrounding bone. The bone undergoes resorption, but seldom is there a remarkable expansion of cortical plats, as in frequently seen in the case of dentigerous cyst.
CONCLUSION:
The present case series reported first and third case after the final diagnosis; treatment was planned as enucleation with curettage along with apicectomy with root canal treated teeth 12. And in the second case after the final diagnosis of infected radicular cyst we have done the surgical enucleation along with extraction of 11, 12, 21, and 22. Cyst formation pathogenesis is a complex process involving a wide spectrum of physiologically active chemicals and their interactions. Therefore, the clinicians should be knowledgeable enough to differentiate types of radicular cyst and available treatment options.
REFERENCES:
- Cysts of the Oral and Maxillofacial Region (4th). Oxford: Blackwell Munksgaard; 2007. Ch. 1
- [CrossRef]
- Radicular cyst masquerading as a multilocular radiolucency. Quintessence Int. 2013;44:71-3.
- [Google Scholar]
- Cysts of the oral and maxillofacial regions (3rd). Boston: Wright; 1992.
- Clinical and radiological features of a large radicular cyst involving the entire maxillary sinus. MUSBED. 2012;2:31-6.
- [Google Scholar]
- Radicular cyst of the anterior maxilla: An insight into the most common inflammatory cyst of the jaws. J Dent Res Rev. 2019;6:26-9.
- [CrossRef] [Google Scholar]
- Radicular Cyst: JKScience. 2009;11(4):187-89.
- The residual radicular cyst: Does it exist? Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;82:471.
- [CrossRef] [PubMed] [Google Scholar]
- New perspectives on radicular cysts: Do they heal? Int Endod J. 1998;31:155 60.
- [CrossRef] [PubMed] [Google Scholar]
- "True" Versus "Bay" Apical Cysts: Clinical, Radiographic, Histopathologic, and Histobacteriologic Features. J Endod. 2020;46(9):1217-1227.
- [CrossRef] [PubMed] [Google Scholar]
- Non-microbial etiology: Periapical cysts sustain post-treatment apical periodontitis. Endod Top. 2003;6:96113.
- [CrossRef] [Google Scholar]
- BMJ Case Rep Published online: [please include Day Month Year]
- [CrossRef]
- Squamous cell carcinoma arising in a residual odontogenic cyst: case report. J Oral Maxillofac Surg. 2005;63:1231-3.
- [CrossRef] [PubMed] [Google Scholar]
- Cystic lesions of the jaws in children. Int J Pediatr Otorhinolaryngol. 2002;62:259.
- [CrossRef] [PubMed] [Google Scholar]







