Translate this page into:
Non-Syndromic Impacted Supernumerary Tooth – A Case Report

* Corresponding author: Dr. Kamatchi M, Department of Paediatric and Preventive Dentistry, Vivekanandha Dental College for Women, Elayampalyam, Tiruchengode, India. kamatchipedo@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Soundarya N, Kamatchi M, Gawthaman M, Indrakumar SP, Kandasamy S, Veerabadhran M. Non-Syndromic Impacted Supernumerary Tooth – A Case Report. Dent J Indira Gandhi Inst Med Sci. 2023;2:134–8. doi: 10.25259/DJIGIMS_8_2023
Abstract
In the field of pediatric dentistry, we encounter plentiful abnormalities in the number, location, dimensions, shape, and eruption of teeth. The most common form is mesiodens, which can be solitary or paired, unerupted or impacted, and frequently lead to complications such as cyst formation, root resorption, rotation, and midline diastema. In the present case, mesiodentes were located in anterior maxilla, one of which erupted and the other was impacted and positioned inverted with respect to 11 that approximated the nasal floor. It was unintentionally detected during radiographic inspection and was surgically removed to prevent any complications. This case description is uncommon and complicated because the impacted mesiodens was positioned in a peculiar nasal location. Cone beam computed tomography was ascertained to be a helpful investigative tool in assessing the correlation of unusually impacted mesiodens to vital structures, thereby providing the best surgical method for its removal.
Keywords
Supernumerary teeth
Impacted mesiodens
Inverted position
Surgical extraction
INTRODUCTION
A developmental anomaly where an extra tooth exists in addition to the normal dentition is known as supernumerary teeth. Though it rarely occurs in the mandible, it can affect both the maxilla and the mandible.[1] The precise etiology of mesiodens is unclear. However, various hypotheses have been proposed, including those involving syndromic diseases, genetic and environmental variables, and disruptions in dental development.[2]
Mesiodens can be classified as conical, supplementary or tuberculate types based on their morphology, with conical being the most common. Mesiodens can exist individually or in groups termed mesiodentes.[2] Mesiodens can either be erupted or impacted and if they remain unerupted they may cause malocclusion.[3] These mesiodens can occasionally cause complications like impaction, delayed eruption, ectopic eruption, crowding, diastema and eruption into the nasal floor, as well as the development of primordial or follicular cysts with bone resorption, pain and swelling with adjacent root resorption and also formation of dentigerous cysts.[3]
Usually asymptomatic, impacted mesiodens is typically found accidentally during routine radiographic examination, because only 25% of the maxillary anterior supernumerary teeth erupt. Therefore, symptoms like asymmetrical pattern of eruption of upper incisors, retained, displaced or rotated incisors and the presence of midline diastema are highly suspected in the case of mesiodens.[4,5]
CASE REPORT
An 8-year-old female patient along with her father reported to the Department of Pedodontics with a complaint of the presence of an additional tooth on the inner side of the upper front tooth region for the past 3 years. The child showed a definitely negative behavior of fearfulness, crying forcefully and extreme negativism (Frankel’s behavior rating scale of 1). On intraoral examination, an extra tooth was noticed on the palatal surface just behind the upper incisors of the maxillary arch [Figure 1 - a, b, c, d, e]. On radiographic examination, orthopantomogram (OPG) as shown in Figure 2 and intraoral periapical (IOPA) radiograph revealed the presence of an erupted supernumerary tooth (mesiodens) in the midline just behind the upper central incisors and more surprisingly, another impacted supernumerary tooth was noted which was seen near the apical region of the upper central incisor just beneath the nasal floor approximating it. On palpation, no eruption bulge of supernumerary tooth was seen on labial and palatal surfaces of the maxillary anterior region. So, a cone beam computed tomography (CBCT) was done to detect the location and position of the impacted supernumerary tooth and its relation with vital structures such as nasopalatine vessels and nerves in axial, coronal, and sagittal planes, and also to endorse the particular position of mesiodens and its close approximation with the maxillary central incisor. CBCT as shown in Figure 3 and exposed impacted mesiodens, which was lying mediolaterally and labial to 11 in an abnormal and inverted position, that is, the apical aspect was facing the root portion of 11 and its incisal aspect was close to the nasal floor. And, it was diagnosed as a mesiodens (erupted and impacted mesiodens). Treatment plan was formulated, which included extraction of the erupted mesiodens under local anesthesia and surgical extraction of impacted mesiodens through maxillary vestibular approach under general anesthesia.

- Intraoral photographs.
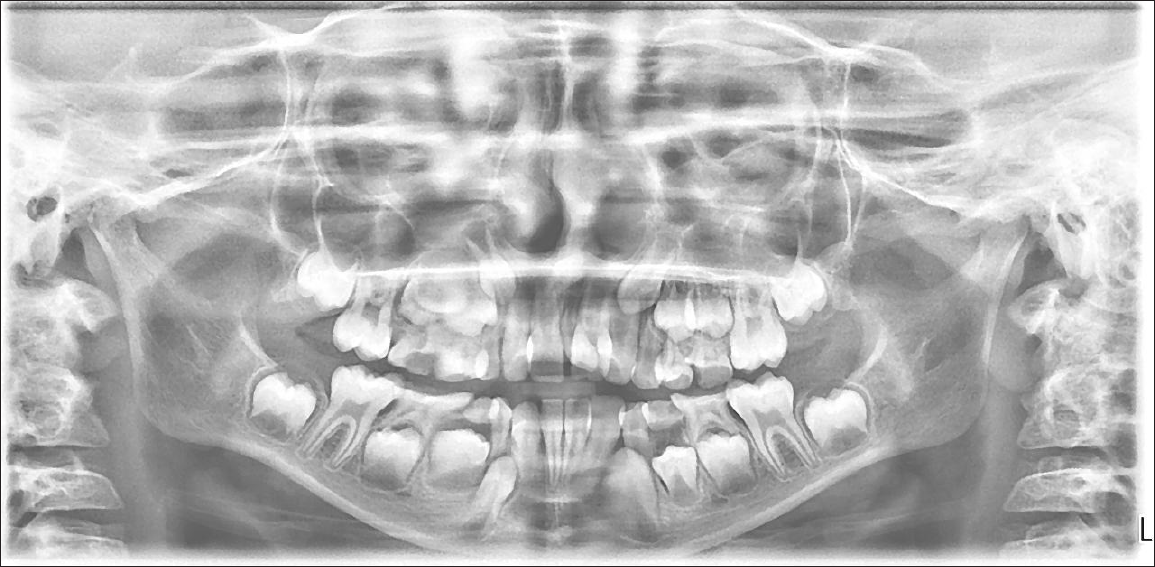
- Orthopantomogram (OPG) of the patient showing impacted and erupted mesiodens in maxillary anterior region.
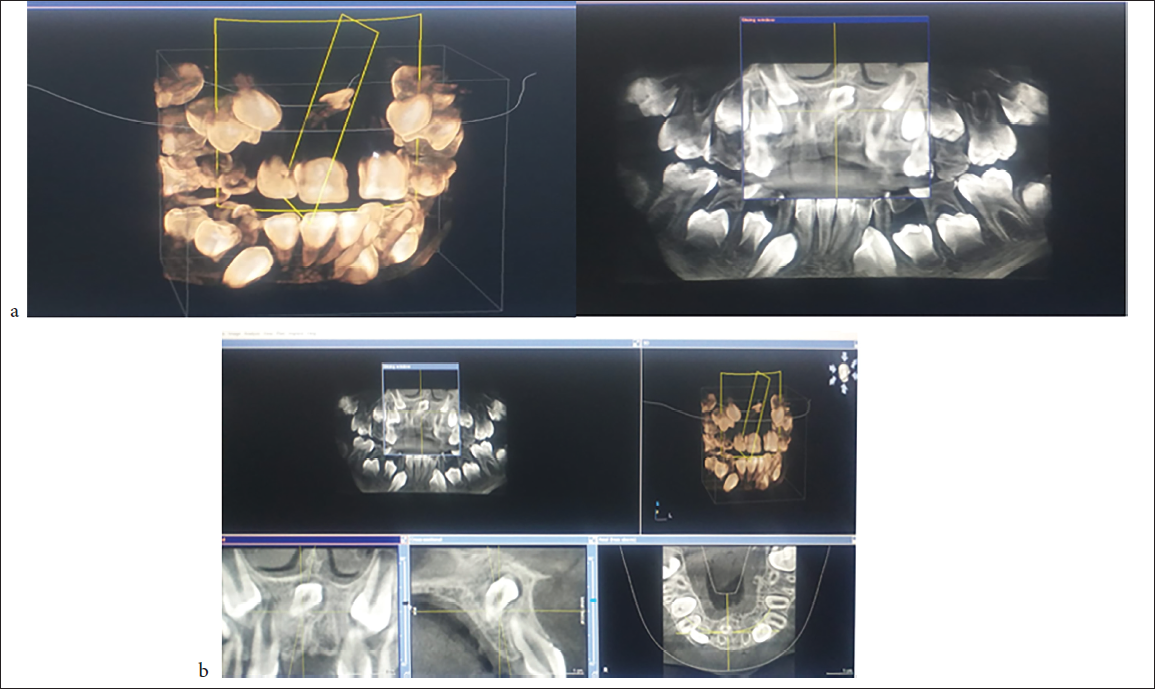
- Cone beam computed tomography (CBCT) images showing impacted mesiodens close to the nasal floor.
Prior to the surgical procedure, informed consent was obtained from the parent. Intra-alveolar extraction (forceps technique) of erupted supernumerary teeth was done. Then, surgical extraction of impacted mesiodens was carried out in a hospital setting under general anesthesia; first an intra-crevicular incision was made from the first premolar to the contralateral first premolar on the labial aspect maxillary anterior region followed by the raising of the mucoperiosteal flap [Figure 4]. Sufficient amount of bone was removed using rotary cutting instruments. The mesiodens was removed as shown in Figure 4 and the extraction socket was checked for any pathological tissue. The flap was relocated and interrupted and figure of eight resorbable sutures were placed in order to approximate the extracted site. The patient was recalled after 2 weeks and healing of the surgically extracted site was found to be satisfactory.
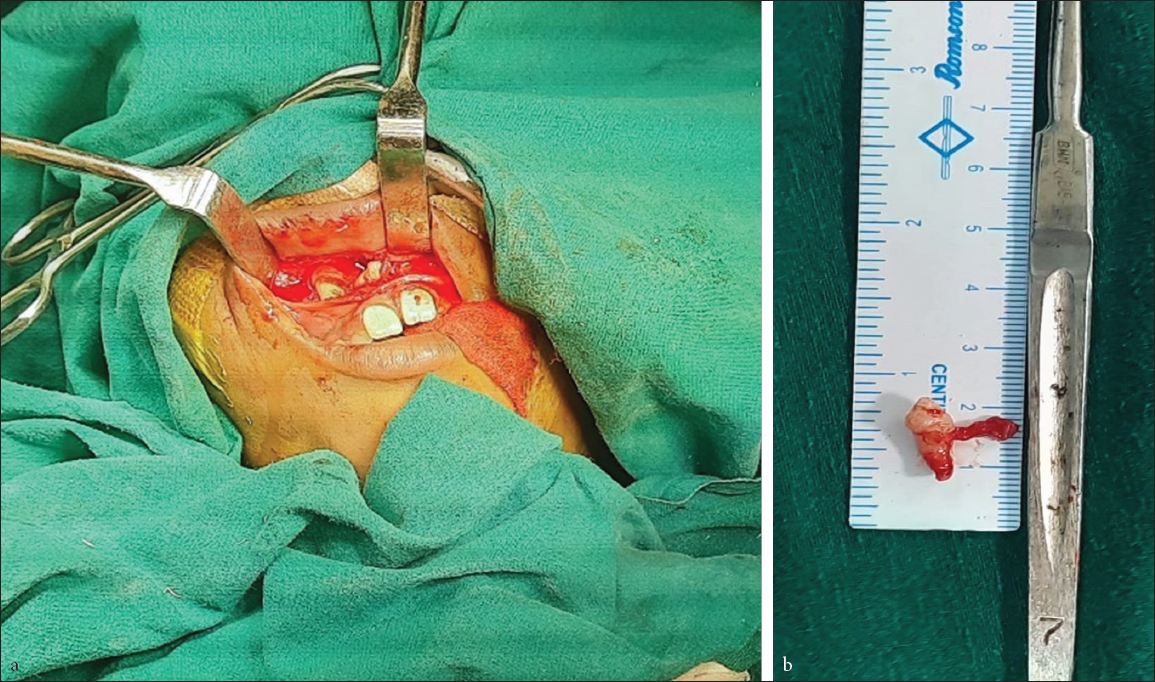
- a) Surgically extracted impacted mesiodens under general anesthesia; b) Mesiodens removed
DISCUSSION
Balk first coined the term mesiodens in 1917 to describe supernumerary teeth that were seen mesial to both central incisors and had a peg-shaped crown. Mesiodens is present in 0.15–1.9% of people.[5] Only 0.1–1% of patients in our community has ectopic teeth or intranasal teeth that erupt into the nasal cavity.[6] It seems that mesiodens is positioned in the floor of the nasal cavity due to varied reasons, including trauma, rhinomaxillary sinusitis, dental conditions, maxillary blisters, obstruction of dental eruption, and trauma to formative tissue. Septal perforation, aspergillosis and naso-oral fistula are some of the most common complications that may occur due to intranasal tooth.[7,8]
Both erupted and unerupted mesiodentes were present in this case, which was quite different from other case reports and unerupted mesiodens show no signs and symptoms. As mentioned earlier, the mesiodens can cause a number of pathological abnormalities, such as granuloma or cyst, having no obvious clinical signs. Young children are more susceptible to these manifestations.[6]
In a case with inverted impacted mesiodens located close to the nasal floor, Sujlana et al. described a trans-nasal approach, while Hauer et al. published a modified maxillary vestibular approach with intranasal dissection for clinical case of inverted impacted mesiodens near the nasal floor.[9,10] But in our case, impacted mesiodens was lying mediolaterally and labial to 11 in an abnormal and inverted position, which was quite different from other cases. Therefore, the maxillary vestibular approach was chosen which is a quite simple surgical technique advocated for our case compared to other clinical cases.
CONCLUSION
The peculiar and challenging feature of this case is the abnormal nasal position of impacted mesiodens. The relation between the unusual position of mesiodens and vital structures, as well as the amount of accessible bone, was determined using CBCT, which was ascertained to be an effective investigative tool in selecting the ideal surgical technique for tooth removal. Consequently, in order to devise an appropriate treatment plan and prevent related complications that requires an early diagnosis, appropriate diagnostic tests and a multidisciplinary strategy are of vital importance.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of Artificial Intelligence (AI)-Assisted Technology for manuscript preparation
The authors confirm that there was no use of Artificial Intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
REFERENCES
- Mesiodens-etiology, prevalence, diagnosis and management. Pak Orthod J. 2013;5:73-6.
- [Google Scholar]
- Surgical management of palatal placed, inverted, dilacerated and impacted mesiodens. Int J Clin Pediatr Dent. 2009;2:30.
- [CrossRef] [PubMed] [Google Scholar]
- Non-syndromic familial mesiodens: Presentation of three cases. Diagnostics. 2022;12:1869.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Management of palatally positioned impacted mesiodens: 2 case reports. J Orthod Endod. 2017;3:1.
- [Google Scholar]
- Transnasal extraction of mesiodens and guided eruption of unusual impacted central incisor: A case report and review of literature. J Clinical Diag Res. 2022;16:ZD10-ZD13.
- [Google Scholar]
- Intranasal inverted tooth: A rare cause of a persistent rhinosinusitis. Indian J Dent Res. 2013;24:762-4.
- [CrossRef] [PubMed] [Google Scholar]
- An inverted impacted mesiodens perforating the nasal floor with an impacted canine. Int J Oral Dent Health. 2019;1:5-6.
- [Google Scholar]
- Modified maxillary vestibular approach with subperiostal intranasal dissection for surgical extractions of mesiodentes impacted in the floor of the nasal cavity. J Craniomaxillofac Surg. 2019;47:1-5.
- [CrossRef] [PubMed] [Google Scholar]








