Translate this page into:
Enamel Hypoplasia – A Clinical Review

Corresponding author: Dr. Rashmi Rokade, Department of Oral Medicine & Radiology, Pandit Deendayal Upadhyay Dental College, Solapur, Maharashtra, India. drrashmi200@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Rokade R, Kulkarni A, Birangane RS, Lahane S, Karkade A, Chitgupkar J. Enamel Hypoplasia – A Clinical Review. Dent J Indira Gandhi Inst Med Sci. 2023;2:109–15. doi: 10.25259/DJIGIMS_7_2023.
Abstract
As a result of congenital and developmental systemic diseases, errors in the growing enamel organ result in enamel abnormalities such as enamel hypoplasia or opacities. The great occurrence of these flaws shows how susceptible teeth are to alterations in the prenatal and postnatal environment.
Enamel hypoplasia contributes to dental caries and tooth wear on teeth because it makes the enamel thinner, more plaque-retentive, and less resistant to acid decomposition than normal enamel. This article explored enamel hypoplasia’s causes and clinical manifestations and presented strategies for managing damaged teeth.
Keywords
Dental fluorosis
Dean’s fluorosis index
enamel
INTRODUCTION
The most frequent flaw in enamel growth and mineralisation is enamel hypoplasia. Enamel, dentin, and cementum are hard teeth tissues created via specific cellular and biochemical mechanisms. Genes govern intricate systems typically triggered by epigenetic, environmental, and environmental variables.[1] Abnormal developmental pathways may contribute to reduced tissue production and poor mineralisation quality.[2] The teeth are the main structures affected if the afflicted genes are expressed primarily in dental tissues, such as the amelogenin gene (AMELX) on enamel.[3] Environmental alterations involving systemic illnesses, hazardous substances, radiation, trauma, and epigenetic factors may exert a consequence on the genetic regulation of enamel and dentin in the manufacturing process.[3]
In instances involving hypoparathyroidism, neonatal tetany, inherited Vitamin D dependency rickets, Vitamin D deficiency rickets, and an array of other perinatal illnesses, the incidence of the lesion is substantially higher. Children in developing nations are particularly prone to linear enamel hypoplasia, a particular type of generalized enamel hypoplasia.[4]
Dental enamel development abnormalities that result from disruption and harm to the enamel organ are known as developmental defects of enamel.[1] A quantitative deficiency known as enamel hypoplasia is characterized by decreased enamel thickness that develops in the secretory stage of amelogenesis.[2]
Hypoplastic or hypocalcified enamel sites can offer the ideal local habitat for cariogenic bacteria to adhere to and establish colonies. These bacteria may persist at the base of the defect in contact with accessible dentin. Therefore, tooth caries might advance swiftly in these regions.[4] Defective enamel is more vulnerable to caries assault because it is more acid-soluble than healthy enamel.[2] This paper aims to summarize current knowledge of genetic and environmental impacts on enamel defects and define how basic science research findings might be applied to the clinic to improve clinical diagnosis of enamel developmental problems.
Assessment indices
To measure dental fluorosis, numerous indices have been created. The Thylstrup and Fejerskov (TF) Index, Dean’s Index (DI), other fluorosis-specific indices and Developmental Defects of Enamel (DDE), a non-specific descriptive index, have also been used to measure fluorosis.[5,6] T-F index is more precise because it is based on a 10-point classification system. Still, the fluorosis index developed by Dean has been used as a gold standard in epidemiological studies.[7]
Dean’s Index (DI) (Dean, 1934)
Dean evaluated the enamel’s clinical appearance that ranged from normal to severe.
Dean recommended evaluating the prevalence and degree of severity in a community named Community Fluorosis Index (CFI) to analyze the severity of dental fluorosis. When the CFI <0.4, Dean considered it of little concern, while indices between 0.4 and 0.6 thresholds and the removal of excess fluoride were indicated when the CFI >0.6 & maximal value of fluoride concentration for esthetic reasons is 0.6 [Table 1].[6]
| Normal | Enamel that is shiny and smooth with translucency |
| Questionable | borderline between normal and very mild. In endemic areas, it may present |
| Very mild | Paper-white areas with small opaque spread irregularly on the buccal & labial side of teeth. |
| Moderate | Pitting on the labial and buccal surfaces, a brownish discoloration and malformation are all evident. |
| Moderately severe | The whole tooth surface is involved with marked pitting & brownish discoloration. |
| Severe | Widespread, dark brown or black areas present |
Assessing enamel defects per Aine
Employing revised Dean’s criteria (1942) along with photographic interpretation, the Indian Council of Medical Research (ICMR) created an index for dental fluorosis in 2013 [Table 2].[3,8]
| Grade | Enamel Defect |
|---|---|
| Grade I |
Chromatic defect present in the enamel. Single or many creams, yellow, or brown opacities without glazing, with distinct or diffuse edges. |
| Grade II |
Minor defects in the structure. Uneven enamel surface with horizontal grooves or shallow pits, probable light opacities, and discolorations |
| Grade III |
Noticeable defects in the structure. A portion of the enamel’s surface, or the entirety of it, may be uneven, filled with deep grooves of varying widths, significant vertical pits, and opacities of different colors or strong discoloration. |
Fluorosis measurement techniques
The traditional approaches for grading fluorosis include direct clinical evaluation and imaging modalities.
Basic clinical examination
The primary explanations for how the clinical examination is employed are simple, quick, economical, and allows for inspecting all tooth surfaces and tactual examination. Nevertheless, the clinical evaluation is primarily related to negative aspects like the examination procedure, the illumination, and the examiner’s bias.
Imaging methods
Imaging techniques have been developed to address these shortcomings in clinical evaluation because they provide a permanent record of the enamel surface for fluorosis estimation. The most significant benefit of implementing imaging techniques is that they lessen the examiner bias and enable repeated measurement by multiple examiners distant from the site of the clinical examination. Essentially, two imaging techniques are utilized to assess fluorosis-traditional and digital photography.
New methods to evaluate fluorosis
Using a 100-millimeter (mm) continuous scale, a Visual Analog Scale (VAS) has been developed based on the esthetic perceptions of images as a legitimate way to assess fluorosis. The best and worst enamel surface spectra were used to ordinate the 100-mm scale. Pretty and colleagues created a new method for preventing these errors by quantifying light fluorescence (QLF), an automated grading system, to evaluate dental fluorosis. The basic concept behind QLF is to contrast variations in fluorescence between sound enamel & unsound enamel (loss of fluorescence intensity in areas of enamel hypomineralisation). The software was used to evaluate the images. The fundamental drawback of QLF is its inability to distinguish mineral loss brought on by fluorosis or other enamel imperfections like caries.[5]
Etiology and Clinical Presentation of Enamel Developmental Defects
Enamel deficiencies are caused by several inherited, acquired, systemic, and local etiological reasons. Since enamel does not change, the flaws record the trauma the enamel organ endured while it matures.
Hereditary conditions
Specific genetic disorders can display enamel deficiencies as a defining characteristic or may be a symptom of a systemic disease. Amelogenesis imperfecta refers to the genetic disorders that only affect the enamel, and the deficiencies may manifest as enamel hypoplasia, hypomaturation, and hypomineralisation.
The main cause of these problems is abnormalities in the amelogenesis-related genes.[1] Enamel hypoplasia may be seen in a variety of genetic medical disorders. In Seckel syndrome, which includes intellectual disability and several skeletal deformities, and Usher syndrome, characterized by sensorineural hearing loss, retinitis pigmentosa, and enamel hypoplasia, enamel defects are frequently observed.[9] Ellis Van Creveld syndrome also exhibits enamel hypoplasia and skeletal and cardiac abnormalities.[10] Additionally, the Treacher-Collins syndrome, the otodental syndrome 22q11 deletion syndrome (velocardiofacial syndrome), and the Heimler syndrome have all been linked to developmental problems.[6]
Acquired conditions
The growing enamel can also be harmed by various systemic or locally acquired diseases during the antenatal, perinatal, or postnatal periods of development and lead to birth abnormalities.[4] The portions of enamel that distinguish the enamel developed during pregnancy from those that form after birth are a common site for developmental abnormalities in the primary dentition.[2] All primary teeth have this zone, also known as the neonatal line, on the crowns, which start to mineralise during prenatally. Depending on how many breakdowns the infant saw throughout the prenatal and neonatal periods, the defect of the neonatal line can range from a bit of alteration in the orientation of the enamel rods to a significant macroscopic defect extending into the dentin.[2] These conditions may be associated with preterm or traumatic births, metabolic or infectious conditions, or environmental exposure to toxic chemicals. As a result, systemic disruptions around birth frequently result in exaggerated neonatal lines that are apparent as enamel hypoplasia in the primary dentition.[2]
Prenatal disorders like maternal vitamin D insufficiency during pregnancy and neonatal tetany may be linked to enamel hypoplasia in the child.[8] Other antenatal factors have been linked to enamel hypoplasia, such as maternal smoking during pregnancy, higher maternal weight gain, and missed opportunities to receive antenatal therapy.[3,10]
Nutritional deficiencies in infants, particularly those related to inadequate intake and absorption of calcium, vitamins A, C, and D, and other nutrients, are known risk factors for enamel hypoplasia in preterm and indigenous populations, despite being uncommon in affluent nations.[3] Furthermore, inadequate nutrition resulting from prolonged breastfeeding without solid supplements has also been put forth as a contributing factor in primary tooth deformities.[2]
Many harmful systemic conditions linked to premature birth, such as respiratory illness, cardiovascular defects, gastrointestinal disturbances, hematological issues, immune deficiency, intracranial hemorrhage, anemia, and renal defects, can be blamed for the developmental defects in low birth weight and preterm children.[3] Developmental deficiencies in the primary dentition have been directly linked to abnormalities related to the mineralisation pathways, including hypocalcaemia, osteopenia, rickets, and hyperbilirubinemia.[8]
Due to the immaturity of the metabolic and mineralisation systems in preterm children, deficiencies in Vitamin D metabolism, mineral levels, and gastrointestinal tract absorption are the main causes of faulty enamel development. Furthermore, the local trauma from laryngoscopy and endotracheal intubation, frequently essential in premature children, often worsens the risks of enamel hypoplasia from systemic disorders.[9] In addition to lack of birth maturity, coeliac disease is another situation where enamel abnormalities can be produced by malabsorption and mineral deficiencies resulting from gut enteropathy carried on by gluten intolerance.[4]
Because many types of renal and hepatic diseases affect the mineralisation pathways, renal and liver disease is also frequently linked to enamel hypoplasia[4] Enamel abnormalities have been linked to infectious diseases brought on by bacteria and viruses, including upper respiratory illnesses, otitis, and infections of the urinary tract.[10] Though congenital syphilis from maternal Treponema pallidum infections is rare in developed nations, it can cause enamel hypoplasia or “notching” of the incisor teeth, and viral infections like chicken pox, rubella, measles, mumps, and influenza has been linked to developmental defects in both primary and permanent dentitions,[3]. At the same time, cytomegalovirus (CMV) has been reported to cause enamel hypoplasia or hypocalcification.[10]
The risk factors for enamel hypoplasia, including maternal or fetal infection, fetal anoxia, and hyperbilirubinemia, are also frequently present in children with cerebral palsy.[10] Various chemicals and medications can cause damage to ameloblasts and result in enamel defects.[9] Children are shown to have enamel hypoplasia of the pitting type due to environmental exposure to lead paint, unintentional or pica ingestion or both.[3] The effects of tetracyclines on tooth discoloration and enamel hypoplasia are well documented. Amoxycillin has recently been blamed for enamel hypoplasia, albeit it can be challenging to ignore the consequences of the infections that necessitate the administration of antibiotics.[9]
In contrast to systemic causes, which typically affect all developing teeth, local variables, including infections and trauma, have also been linked to enamel hypoplasia adjacent to the damage.
Fluorosis is a condition that should be periodically evaluated since it reflects the amount of fluoride consumed during the enamel’s development. When fluorosis disease has been determined to be significant, a community should reduce the amount of fluoride ingested by children with developing teeth.
Amelogenesis Imperfecta
Additionally, known as Hereditary Enamel Dysplasia, Hereditary Brown Enamel, and Hereditary Brown Opalescent Teeth.
Depending on the clinical appearance of the anomalies and the expected stage of enamel production that is most affected, it can be divided into four major groups [Figure 1].
-
⮚
Type I- hypoplastic enamel (the most common one)
-
⮚
Type II-hypomaturated enamel
-
⮚
Type III-hypocalcified enamel
-
⮚
Type IV-hypo maturated-hypoplastic enamel with taurodontism.[8]

- Autosomal dominant inheritance with smooth hypoplastic amelogenesis imperfecta (AI).
Depending on the quantity of enamel present on the tooth and the amount of wear on the occlusal and incisal side, the form of the tooth may be normal or irregular. The enamel may be completely missing or visible on the radiograph as a thin layer, mostly over the interproximal area and along the edges of the cusps. Whenever the calcification has been seriously damaged, it often appears to have nearly the same radiopacity as the dentin, making it difficult to distinguish between the two [Figure 1].
Environmental Enamel Hypoplasia
Enamel hypoplasia is an incomplete or defective formation of the organic enamel matrix of teeth.[11]
There are two varieties of enamel hypoplasia:
-
Imperfect amelogenesis as a hereditary form.
-
A condition brought on by external/environmental factors.
In the hereditary type, deciduous and permanent dentitions are typically involved; typically, only the enamel is damaged. However, in the environmental variety, any dentition may be involved, and occasionally, only one tooth will be affected, at least partially, by both enamel and dentin [Figure 2][12].

- Environmental enamel hypoplasia.
If the insult happens while the enamel is still in the formative stage, hypoplasia will result. There can be no more enamel defects when the enamel has calcified. If the condition is more severe, the enamel may have rows of deep pits distributed horizontally over the tooth’s surface. In mild environmental hypoplasia, just a few minor grooves, pits, or fissures are present on the enamel surface. A single row of pits or multiple rows of pits implies multiple injuries. In severe cases, a sizable enamel section may be missing, indicating a protracted disruption in the ameloblasts’ functionality.[11]
Hypoplasia due to Nutritional Deficiency and Exanthematous Fever
Rickets is the most frequent cause of enamel hypoplasia when teeth are forming. Exanthematous illnesses, including measles, scarlet fever, and chicken pox, are the main contributing causes. Because ameloblasts are one of the body’s most metabolically sensitive cell types, it can be stated that any severe systemic illness nutritional deficit can potentially cause enamel hypoplasia.
These inadequacies typically result in hypoplastic teeth that are pitting in appearance. The teeth’s clinical appearance may be unhealthy, and the pits frequently discolorate. The teeth most usually affected are the central and lateral incisors, cuspids, and first molars. Other instances only have the central incisor, cuspid, and first molar because the cuspid’s tip forms before the lateral incisor. Rarely are premolars, second, or third molars malformed.[11]
Congenital syphilis-related enamel hypoplasia
Congenital syphilis-related hypoplasia has a pathognomonic appearance. The permanent incisors and first molars on the maxilla and mandible are involved. The molars have been referred to as “mulberry molars” (Moon’s molars, Fournier’s molars), whereas the affected anterior teeth are referred to as “Hutchinson’s teeth” [Figure 3].[11,13] The form of the upper central incisor is distinctively “screw-driver” shaped. Furthermore, the incisal edge is typically notched. Congenital syphilis first molars have irregularly shaped crowns and enamel arranged more like a mass of globules on the occlusal surface and the occlusal third of the tooth than well-formed cusps [Figure 4]. The crown is smaller on the occlusal surface than the cervical edge.[11]

- Hutchinson’s teeth.

- Mulberry molars.
Hypocalcemia-related enamel hypoplasia
Reducing blood calcium levels brings on Tetany, but other medical disorders can also bring it on. Vitamin D deficiency is the most frequent cause, and parathyroid deficiency (para thyroprivic tetany) is a possibility. In tetany, the serum calcium level can drop as low as 6-8 mg per 100 ml; at this level, teeth developing synergistically frequently experience enamel hypoplasia. In most cases, these are of the pitting type of enamel hypoplasia [Figure 5][14].

- Enamel hypoplasia due to vitamin D deficit.
Enamel hypoplasia due to birth injuries
It is a form of hypoplasia because the enamel and dentin are disturbed, indicating trauma or a change in the environment at birth.
Localized infection or trauma-related enamel hypoplasia
It’s an uncommon form of hypoplasia that only infrequently affects one tooth, most frequently one of the permanent maxillary incisors or a maxillary or mandibular premolar. Turner’s tooth is the common name given to these single teeth, while Turner’s hypoplasia is a term for them [Figures 6 and 7].[11,12]
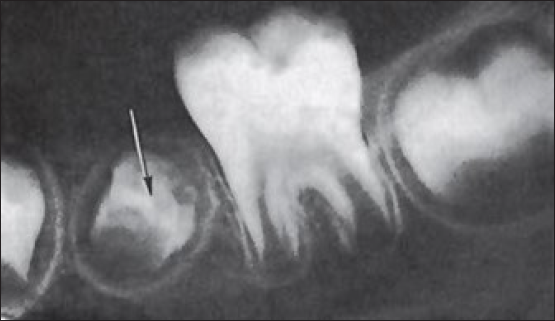
- Turner’s tooth-defect in quality and thickness of the enamel (black arrow) Radiographic image.

- Turner’s hypoplasia - Clinical Image.
Mottled Enamel (Enamel Hypoplasia related to Fluoride)
It is now well-regarded that the intake of fluoride-containing drinking water around the time of amelogenesis may result in mottled enamel. Mottling of teeth is clinically evident at a level above 0.9–1.0 part per million of fluoride in the water.
Wide area of severity in the presentation of mottled teeth, differing from (1) questionable changes characterized by occasional white spotting or flecking of the enamel, (2) mild changes characterized by white opaque spots involving more of the tooth surface area, (3) moderate and severe changes showing pitting and brownish discoloration of teeth, (4) a corroded appearance of the teeth [Figure 8].

- Environmental enamel hypoplasia secondary to dental fluorosis; white, chalky opacities and brownish discoloration are present, along with pitting on the labial aspect.
Hypoplasia related to Idiopathic Factors
Various circumstances have reportedly caused enamel hypoplasia, although even in cases with thorough histories, the majority are thought to be unrelated. The causative agent may have been some sickness or systemic disturbance so light that it had no noticeable effects on the patient in cases where the etiology could not be confirmed. Ameloblast is a susceptible type of cell and is readily damaged.[11]
Conclusion
Numerous genetic and acquired etiological factors can cause enamel hypoplasia that can lead to dental hypersensitivity and impoverished esthetics. The adverse consequences of enamel hypoplasia include an increased risk of tooth wear and dental caries. Enamel protection strategies and efficient preventative treatment and monitoring require attention. Dentists must consider these patients’ social needs and intervene to alleviate their suffering. Consequently, this article aims to better clinicians’ understanding of the clinical diagnostic needed for this type of condition.
Declaration of Patients Consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest
Use of Artificial Intelligence (AI)-Assisted Technology for manuscript preparation
The authors confirm that there was no use of Artificial Intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
REFERENCES
- Developmental enamel defects in the primary dentition: Aetiology and clinical management. Aust Dent J. 2013;58:133-40.
- [CrossRef] [PubMed] [Google Scholar]
- Association between enamel hypoplasia and dental caries in primary second molars: A cohort study. Caries Res. 2009;43:345-53.
- [CrossRef] [PubMed] [Google Scholar]
- Comparative evaluation of three different recording criteria of dental fluorosis in a known endemic fluoride area of Haryana. Indian J Med Res. 2018;147:567.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The etiology of enamel hypoplasia: A unifying concept. J Pediatr. 1981;98:888-93.
- [CrossRef] [PubMed] [Google Scholar]
- Enamel hypoplasia or amelogenesis imperfecta restorative approach. Brazilian J Oral Sci. 2006;5:941-3.
- [Google Scholar]
- Methods and indices in measuring fluorosis: A review. Arch Orofacial Sci 2017:77-85.
- [Google Scholar]
- Prevalence of dental fluorosis and associated risk factors in Allappuzha district, Kerala. Natl Med J India. 1999;12:99-102.
- [PubMed] [Google Scholar]
- Dental enamel defects and dental maturity in children and adolescents with coeliac disease. Proc Finn Dent Soc. 1986;82:1-7.
- [PubMed] [Google Scholar]
- Clinical evaluation of dental enamel defects and oral findings in coeliac children. Eur Oral Res. 2018;52:150-6.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Enamel hypoplasia and its role in identification of individuals: A review of literature. Indian J Dent. 2015;6:99.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Shafer’s textbook of oral pathology. India: Elsevier; 2009.
- Oral and maxillofacial pathology. Elsevier Health Sciences; 2015.
- Validation of ICMR index for identification of dental fluorosis in epidemiological studies. Indian J Med Res. 2016;144:52.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Dental manifestations of dermatologic conditions. J Am Acad Dermatol. 2009;60:289-98.
- [CrossRef] [PubMed] [Google Scholar]







