Translate this page into:
Comparing Different Techniques for Uncovering Dental Implants during Second-Stage Surgery: Tissue Punch versus Laser versus Electrosurgical Unit

*Corresponding author: Dr. Dayakar M M, Department of Periodontology and Oral Implantology, KVG Dental College & Hospital, Kurunjibhag, Dakshina Kannada, Sullia, Karnataka, India. mmdayakar@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: MM D, H P. Comparing Different Techniques for Uncovering Dental Implants during Second-Stage Surgery: Tissue Punch versus Laser versus Electrosurgical Unit. Dent J Indira Gandhi Int Med Sci. 2024;3:108-111. doi: 10.25259/DJIGIMS_12_2024
Abstract
There are multiple ways to modify soft tissue to reveal dental implants and start the prosthetic phase of treatment. Historically, the soft tissue has been sliced to reveal the underlying implant for the restorative phase using devices like a tissue punch or scalpel blade. Three methods are available for doing it: electrocautery, lasers, and scalpels. Lasers and electrocautery have gained popularity as more dentists choose to experiment with contemporary technologies. It’s challenging to decide between a laser and electrocautery, though. In this clinical report, many modalities are used, and the benefits and drawbacks of each are discussed.
Keywords
Tissue punch
Laser
Electrosurgical unit
Implants
INTRODUCTION
Using an implant-supported restoration to restore the edentulous space requires at least three to four clinical steps. Following preoperative analysis, the dentist implants the chosen dental implant in the patient during the initial clinical procedure, often known as the surgical phase.[1–3] Once effective osseointegration has been verified by radiography, the implant is subsequently exposed at the second clinical session in accordance with the conventional healing procedure. After the implant has been exposed, a healing cap, often referred to as a gingival former, is screwed onto it. It is left in place for 48 hours to allow the soft tissue around the healing abutment to heal and take up the contour of the soft tissue around it, which later on produces an aesthetic emergence profile.[4,5] Following this clinical visit, the patient is summoned back for the third step (the impression/prosthetic phase), during which the impressions for the final restorations are prepared. Electrosurgery or laser has been proposed as a blade substitute that can cauterize the cut edges and lessen bleeding after surgery.
The literature lists three commonly used techniques for revealing the submerged implant.[6,7] The traditional method uses a scalpel, while current technology uses electrosurgery and lasers to expose the implant. The operator prefers to make incisions.
Lasers and electrosurgery are two examples of modern technology in action.[8] Many operators still prefer scalpels since they are readily available in even the most basic operatories. Simple to use, affordable and quite quick and smooth recovery are some of the other justifications for the widespread and ongoing usage of scalpels. Its drawbacks include blood at the surgical site, numerous needless cuts or incisions/exposure, and impaired operatory site visibility.[9] Consequently, it makes sense for operators to use modern bloodless fields for surgical procedures if the equipment needed is conveniently located in the operatory.[10]
The optimal technique for soft tissue cutting – laser or electrosurgery – remains up for debate.
Case 1
A 41-year-old male patient presented with a missing mandibular right first and second molar due to decay [Figure 1]. After discussing all of the possible outcomes for the lost tooth, the patient chose to proceed with implant placement. Following regular protocol, a titanium implant was placed, and months later, the patient was called back for prosthetic rehabilitation.
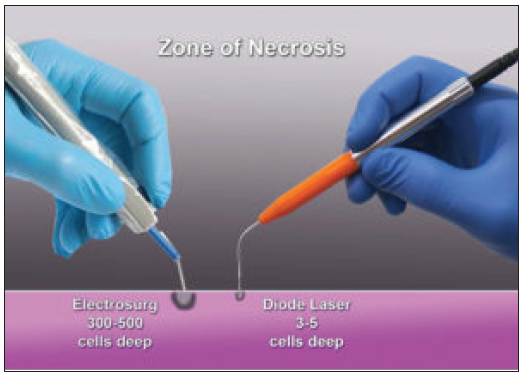
- Comparison of depth of the zone of necrosis of an electrosurgical unit and diode laser.
For the second stage of surgery, it was decided to expose the implant with 46 sides using an electrosurgical unit, and a wrt 47 diode laser was used to expose it using electrosurgical unit [Figures 2–3]. Electrosurgery has been proposed as a blade substitute that can cauterize the cut edges and lessen bleeding after surgery. Deeper penetration is achieved by electrosurgery, which affects 300–500 cell layers below the surface. This, together with the temperature rise noted at the incision site, causes tissue to shrink. As a result, healing must occur for at least two weeks before an impression can be made to ensure that the gingival edge is in a stable position. A general recommendation is to avoid electrosurgery around dental implants.
![Implant sites are exposed using an electrosurgical unit (immediate post-op) wrt 46 and a doide laser wrt 47 [C 1].](/content/163/2024/3/2/img/DJIGIMS-3-2-108-g3.png)
- Implant sites are exposed using an electrosurgical unit (immediate post-op) wrt 46 and a doide laser wrt 47 [C 1].
![Implant sites exposed using electrosurgical unit (after 14 days) wrt 46 and diode laser wrt 47 [C 1].](/content/163/2024/3/2/img/DJIGIMS-3-2-108-g4.png)
- Implant sites exposed using electrosurgical unit (after 14 days) wrt 46 and diode laser wrt 47 [C 1].
Initially, when we think of lasers, we picture cutting instruments, particularly those used on soft tissues. When used within the acceptable temperature range, lasers have the potential to modify soft tissue inside and around dental implants for healing or to change the gingival margin for aesthetic purposes without adversely affecting the surrounding bone. Furthermore, coagulation may be regulated so that impressions can be made at the moment of uncovering without worrying about blood compromising the accuracy of the gingival component of the record. Tissue shrinking is not an issue because, in contrast to an electrosurgery unit, cutting the tissue with the diode does not influence the deep layers of cells in the gingiva.
Water, pigmentation, melanin, and hemoglobin all absorb diode laser energy. The diode laser does not affect dentin, enamel, or titanium because these materials don’t contain these substances. Nevertheless, these components are present in gingival tissue, and the diode offers the advantages of improved sterilizing, coagulation, and cutting within the soft tissue at the laser contact site. The advantages of the diode laser over the electrosurgical unit include faster healing durations since fewer cells are damaged and more precise outcomes because of a substantially decreased zone of necrosis at the contact (zone of necrosis for the diode laser = 3–5 cells deep, whereas for electrosurgery it is 300–500 cells deep), which results in reduced tissue shrinkage during healing and the removal of tissue charring (common when electrosurgery is utilized).
Case 2
The mandibular right first molar of a 24-year-old male patient was gone as a result of deterioration [Figure 4]. After considering all available treatment options, the patient chose to proceed with implant insertion for the lost tooth.
![Implant site exposed using tissue punch biopsy (after 14 days) wrt 46 [C 2].](/content/163/2024/3/2/img/DJIGIMS-3-2-108-g5.png)
- Implant site exposed using tissue punch biopsy (after 14 days) wrt 46 [C 2].
During second-stage surgery, an implant might be uncovered in a few different ways. A tissue punch, a diode laser, or a #15 blade can all be used. It depends on how well the dentist places the implant and where the associated tissue should be positioned.
DISCUSSION
A tissue punch can be the best choice if you are certain of the implant’s buccolingual and mesiodistal locations and there is plenty of connected tissue. It is a very quick operation that eliminates flaps and enables the healing collar to be placed in a matter of minutes. However, the warning with this method is the possibility of significant issues if an error exceeds one millimeter. Either you’d have to pull a second blow or take out the scalpel. If you can’t work the remaining tissue to cover the exposed bone, this could lead to exposed bone and secondary healing. A diode laser can be used to achieve the same result as the tissue punch while hastening the healing process of the injured tissue.
CONCLUSION
When soft tissue modification has to be done or to expose dental implants or aesthetically recontour the gingival margin, diode lasers are a helpful addition, keeping the temperature profile within the bone’s safe range and offering more safety than electrosurgery. They also don’t shrink tissue, which could have an impact on the final aesthetic result. When compared to using a scalpel or tissue punch, the diode tip gives a distinct benefit since it allows for simultaneous cutting and coagulation (hemostasis), allowing for quick imprints without compromising the accuracy of the acquired soft tissue contours and position.
Ethical approval
The Institutional Review Board has waived the ethical approval for this study.
Conflicts of interest
There are no conflicts of interest
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that they have used AI-assisted technology for assisting in the writing or editing of the manuscript or image creations.
REFERENCES
- Single-stage implant surgery using a tissue punch. J Oral Maxillofac Surg. 2000;58:456-7.
- [CrossRef] [PubMed] [Google Scholar]
- Use of electrosurgery and lasers in the presence of dental implants. Int J Oral Maxillofac Implants. 2001;16:578-82.
- [PubMed] [Google Scholar]
- Effects on oral soft tissue produced by a diode laser in vitro. Laser Surg Med 1999:401-6.
- [CrossRef] [Google Scholar]
- Efficacy and safety of a diode laser in second-stage implant surgery: A comparative study. Int J Oral Maxillofac Surg. 2014;43:633-8.
- [CrossRef] [PubMed] [Google Scholar]
- Uncovering the tooth: The diode laser to uncover teeth, brackets and implants. Dent Today. 2012;31:168.
- [PubMed] [Google Scholar]
- The use of an 980-nm Diode and 1064·nm Nd:YAG Liaser for Gingival Retraction in Fixed Prosthsis/Oral Laser Applications. . 2004;4:183-90.
- [Google Scholar]
- Using a diode laser to uncover dental implants in second-stage surgery. Gen Dent. 2005;53:414-7.
- [PubMed] [Google Scholar]
- Periodontal and peri-implant wound healing following laser therapy. Periodontol 2000. 2015;68:217-69.
- [CrossRef] [PubMed] [Google Scholar]
- The diode laser – The diode laser in second stage implant recovery. Dent Today. 2011;30:144.
- [PubMed] [Google Scholar]
- Laser applications in oral surgery and implant dentistry. Lasers Med Sci. 2007;22:217-21.
- [CrossRef] [PubMed] [Google Scholar]







