Translate this page into:
The Role of Arthroscopy in Treating Temporomandibular Joint (TMJ) Disorders: A Comprehensive Literature Review

*Corresponding author: Subia Ekram, Department of Oral and Maxillofacial Surgery and Oral Implantology, Dental Institute, Rajendra Institute of Medical Sciences, Ranchi, Jharkhand, India. subia.ekram786@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Noorani MK, Tigga C, Ekram S. The Role of Arthroscopy in Treating Temporomandibular Joint (TMJ) Disorders: A Comprehensive Literature Review. Dent J Indira Gandhi Int Med Sci. 2024;3:13–9. doi: 10.25259/DJIGIMS_17_2023
Abstract
This study was meant to analyze the advantages and limitations of various temporomandibular joint (TMJ) arthroscopy techniques and adaptations outlined in the existing literature. Arthroscopy has emerged as a valuable tool within oral and maxillofacial surgery for diagnosing and treating temporomandibular joint disorders (TMDs). Its noteworthy attributes encompass the ability to perform targeted biopsies simultaneously with minimal and infrequent complications, leading to a notably elevated accuracy in TMD diagnosis. Moreover, the integration of surgical lasers into TMJ arthroscopy has heightened the viability of this surgical approach, resulting in favorable immediate outcomes while maintaining cost-effectiveness. Lastly, the realm of arthroscopy presents unique avenues for research, offering insights into the intricate etiopathogenesis of TMD.
Keywords
Arthroscopy
Temporomandibular joint disorders
Temporomandibular joint
INTRODUCTION
Arthroscopy, which is derived from the words “joint” and “to view,” simply means looking into a joint. Temporomandibular joint (TMJ) arthroscopy is an excellent diagnostic tool complementing clinical and radiological examinations.[1] Arthroscopy is a relatively safe and conservative procedure with few complications, but a difficult technique to learn.[2] Dr. Ohnishi introduced arthroscopy of the TMJ in 1974 ,and its possibilities were described in the Japanese literature in 1975, [3–6] and he applied it clinically to patients with osteoarthritis and internal diseases. Subsequently, TMJ arthroscopy progressed from being a diagnostic tool to an operative intervention for individuals with TMJ disorders. This technique quickly gained global recognition and acceptance. During the late 1990s, a plethora of articles and publications emerged, concentrating on the subject of TMJ arthroscopy. Arthroscopy-related literature,such as intra-articular pathology and synovial fluid analysis, contributed to the advancement of biological basis of TMJ arthroscopy. In 1995, Milam and Schmitz scrutinized the rationale and importance of molecular pathological sequences within the synovial fluid of individuals with TMJ conditions. They presented a hypothesis and proposed several conceivable pathways.[7] Compared to an open dissection technique, the anatomy seen through an arthroscopy is somewhat different. The anterior, intermediate, and posterior synovial recesses upper joint cavities. The arthroscopic examination allows visualization of distinct regions within the upper joint cavity, including the posterior synovial recess, intermediate zone recess, and anterior synovial recess. The anterior and posterior bands of the disc, along with the articular eminence in the intermediate zone, are observable. Synovial membranes cover nonfunctional aspects of the joint, while connective cartilage overlays the joint surfaces. The disc is primarily composed of dense fibrous connective tissue. The lower joint space is typically not observed in routine arthroscopy, unless there is disc perforation during the procedure.
INDICATIONS FOR TMJ ARTHROSCOPY
Patients experiencing pain and jaw dysfunction that have not responded to non-surgical dental or medical management.
Individuals with frequent mandibular dislocation.
Persistent atypical facial pain in the preauricular region.
Cases of osteoarthritis affecting the TMJ.
Posttraumatic complaints related to the TMJ.
Conditions involving pseudotumors.
Biopsy of suspected lesions or diseases within the TMJ.
Confirmation of diagnostic findings that suggest the need for surgical intervention.
CONTRAINDICATIONS TO TMJ ARTHROSCOPY
Advanced bony and fibrous ankylosis.
Ankylosing osteoarthritis.
Presence of malignant tumors.
Significant resorption of the glenoid fossa.
Elevated risk of hemorrhage, which could lead to hemarthrosis.
Active skin infection in the area, as puncturing through infected skin may result in septic joint complications postoperatively.
EQUIPMENT
An arthroscope is a rigid cylindrical device equipped with internal lenses, facilitating a broader and brighter field of view as shown in Figure 1. Ideally, it should possess a diameter of less than 2 mm and a field of view of 30 degrees. A 1.9 mm arthroscope typically includes a C-mount (a) a focusing ring (b), and a light source attachment (c) as shown in Figure 2.

- Armamentarium for arthroscopy.
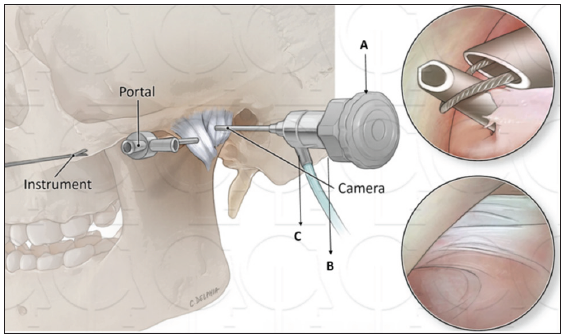
- A: 1.9-mm arthroscope with C-mount attachment, B: focusing ring, and C: light source attachment.
The essential components of an arthroscope are as follows:
Arthroscopy Sheath: This tool guides the arthroscope into the joint space during the procedure.
Trocar: Employed in arthroscopic surgery, the trocar is utilized to puncture the lateral capsule of the socket.
Cannulas: Cannulas serve the purpose of directing manual instruments into the joint, as well as facilitating irrigation and drainage. The diameter of devices inserted into the cannula, such as points, should be at least 0.1 mm smaller than the inner diameter of the cannula. Markings on the cannulas enable the surgeon to regulate the depth of insertion, providing control over the penetration depth.
Classification of TMJ Arthroscopy: TMJ arthroscopy can be categorized into two types:
Diagnostic Arthroscopy: Involving a single puncture, this type serves for diagnostic purposes and basic interventions.
Therapeutic Arthroscopy: Utilizing multiple punctures, therapeutic arthroscopy is capable of performing complex surgical procedures.
Surgical Technique: The arthroscopic approach is through the TMJ, involving the following steps:
Infiltration of the upper joint space with bupivacaine, refer to Figure 3.
Identification and marking of the tragus center.
Determination and marking of the lateral canthus of the eye.
Drawing a straight line connecting the center of the tragus to the lateral canthus.
Measurement and marking of a point 10 mm from the center of the tragus, designating point A, located 2 mm below it. A trocar with an obturator is positioned at this point, and the obturator is then removed to facilitate arthroscope insertion [Figure 4].
Measurement and marking on the original line 20 mm from the center of the tragus. Perpendicular to this point, a line is drawn, and 10 mm below it, point B is marked for the insertion of the trocar with the sharp obturator.
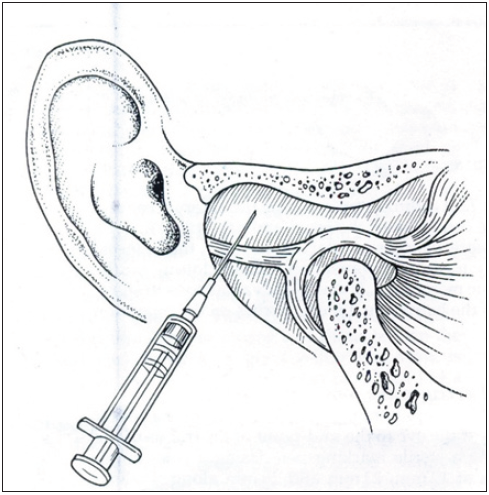
- Distension of upper joint space with bupivacaine.

- Trago-canthal line measurements; posterolateral, middle lateral, and anterolateral puncture points.
There are various approaches described for TMJ arthroscopy.
Superior posterolateral approach
Inferior posterolateral approach
Superior anterolateral approach
Inferior anterolateral approach
Endaural approach
Examine the external ear before performing TMJ arthroscopy, and observe the canal and drum condition. To stop blood from clotting on the tympanic membrane, insert a tiny piece of Jelonet or tulle gras into the external auditory meatus. Local anesthesia can be used for diagnostic examination, lysis, and lavage, but these procedures typically call for intravenous sedation. For arthroscopic procedures, few surgeons prefer general anesthesia.
VARIOUS TECHNIQUES FOR TMJ ARTHROSCOPY
Superior Posterolateral Approach
In this technique, the mandible is displaced downward and forward, resulting in the formation of a triangular depression in front of the tragus. This concavity is characterized by the upper boundary constituted by the glenoid fossa, the front-lower boundary by the dorsal aspect of the condylar head, and the rear boundary by the external auditory canal. The trocar is then introduced at the apex of this depression, positioned just above the surgeon’s gloved fingertip outlining the lower part of the glenoid fossa.
The trocar is maneuvered in an anterosuperior direction, directed toward the posterior incline of the eminentia. This particular approach facilitates access to the upper posterior joint space, providing a visual of the upper joint space. However, challenges may arise concerning visualization, particularly when observing the synovial pouch in the upper frontal area and the synovial groove in the inner paradiscal region [Figures 5–8].
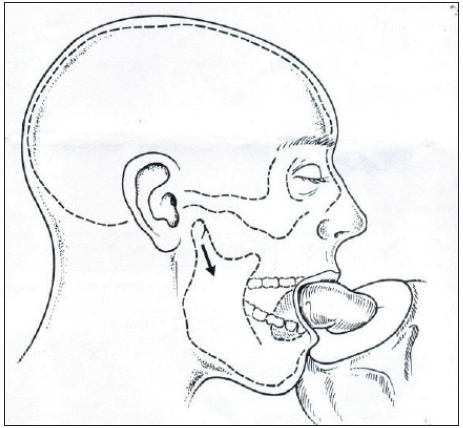
- Condylar Head distracted laterally to stretch lateral capsule, black arrow indicates Condylar Head distracted laterally.
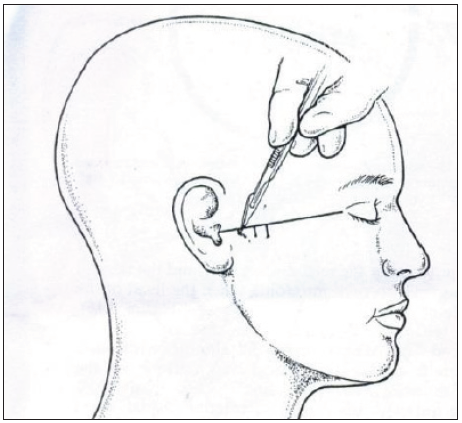
- Optional stab incisions.
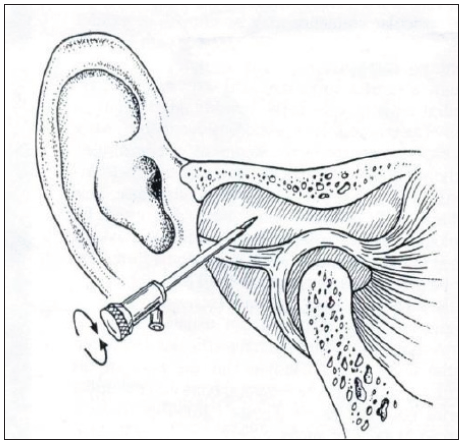
- Posterolateral puncture with rotatory movements of sharp trocars and cannula, two rotating arrows denotes the rotatory movement.
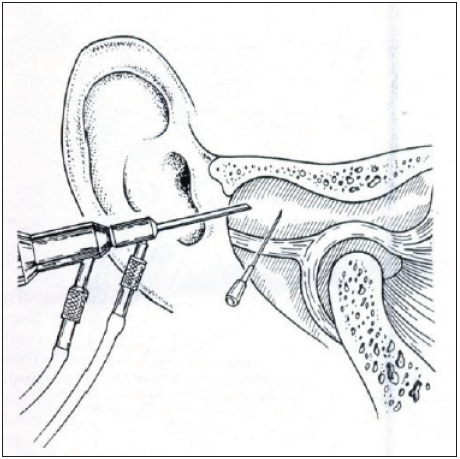
- The arthroscope slides down the cannula and is connected to the irrigation extension tube. A21G needle is inserted for outflow via the 22/6 mm lateral puncture point.
Inferior Posterolateral Approach
This approach represents a modification of the inferolateral technique, directing the trocar toward the lateral and posterior surface of the mandibular head. This adjustment allows for the examination of the synovial pouch located beneath and behind, as well as the posterior aspect of the condylar head.
Superior Anterolateral Approach
In this approach, the trocar is directed upward, backward, and inward along the lower slope of the articular eminence, utilizing the prominence of the lateral articular tubercle as a reference point. The mandibular condyle is repositioned by the surgical assistant, gently moving it downward and backward.[8] This method facilitates instrumentation or visualization of the front-upper compartment of the joint.
Inferior Anterolateral Approach
This approach presents greater technical complexity compared to the previously discussed methods. It allows for the visualization of the synovial pouch located in the lower frontal region. This technique involves the examination of both the condylar head and the articular tubercle. The trocar is then inserted in a position located in front of the lateral extremity of the condylar head and just beneath the articular tubercle. This situates the trocar within the synovial pouch in the lower frontal area, positioned closely to the anterior aspect of the condylar head. This approach facilitates the examination of the synovial pouch in the lower frontal region.
Triangulation
Analyzing the anterior slope of the articular eminence presents difficulties, and to reach the upper joint space, the operator needs to utilize the 29/7 mm point. This is accomplished by introducing a second trocar and cannula while maintaining the position of the initial cannula, as illustrated in Figure 9.

- Triangulation using two separate portals of entry.
ENDAURAL APPROACH
Steps of the Endaural Approach
Introduction of heparinized Ringer’s lactate to expand the joint.
Placement of an outflow needle in the front-lateral region of the joint.
Arthroscopic examination of the joint utilizing the inferolateral technique [Figure 10]. The procedure initiates with the insertion of a trocar into the upper posterior joint space, positioned approximately 1–1.5 cm towards the inner side of the tragus’s outer edge, traversing through the anterior wall of the external auditory canal.[9] The trocar is directed in an anterosuperior trajectory, slightly towards the inner side of the posterior slope of the eminentia. This method permits access to and visualization of the upper posterior joint space, including the medial and lateral troughs in the paradiscal region.
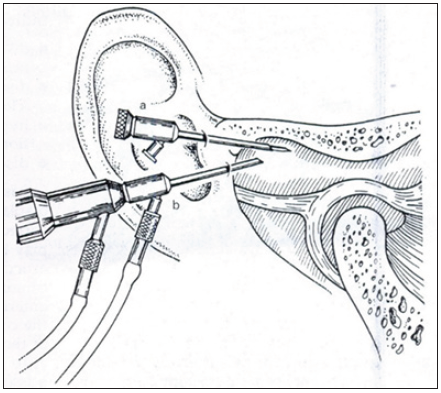
- Endaural triangulation of the posterior superior “pouch.” pouch, a: endaural cannula and trocar, b: posterolateral arthroscope.
Complications
Overall, TMJ arthroscopy is a procedure with a favorable safety procedure. It is minimally intrusive and can be conducted on an outpatient basis. Nevertheless, potential complications do arise. These encompass risks such as facial nerve injury, arthrofibrosis, infection, and the possibility of perforating into the ear canal, tympanic membrane, or even causing subdural or epidural hematoma by breaching the middle cranial fossa. Nonetheless, by employing meticulous surgical techniques, careful attention, and appropriate postoperative rehabilitation tailored to the specific procedure, these complication rates can be nearly eliminated.
DISCUSSION
TMDs present us with very intricate and complex issues that can make diagnosis and treatment challenging. Proper patient selection forms a crucial basis for achieving successful surgical outcomes. The primary reason for undergoing TMJ surgery is when there’s a type of dysfunction in the cranio-mandibular system that stems from issues within the articular disc and the tissue behind it.
The American Association of Oral and Maxillofacial Surgery (AAOMS)[10] recognizes five main indications for arthroscopy:
Internal derangement (ID) of the TMJ, mainly Wilkes stages II, III, and IV
Degenerative joint disease
Synovitis
Recurrent dislocation of the jaw joint due to disc displacement or painful excessive movement of the joint
Hypomobility caused by intra-articular adherences
To get good results with TMJ arthroscopy, it is important to take surgical medication. It’s debatable whether prophylactic antibiotics should be used to stop postoperative infection. Due to the low incidence of infection after arthroscopy procedures, there is an absence of good prospective studies in the orthopedic literature. There is no advisory statement on the subject from the American Academy of Orthopedic Surgeons. However, there is literature that essentially states that healthy patients should not take antibiotic prophylaxis for arthroscopic procedures. These authors believe that those who are prone to infection should take antibiotics. Individuals with diabetes, weakened immune systems, or skin conditions are among them. Administering 1 g of intravenous cefazolin 1 hour before the procedure provides effective protection for managing these patients preventively when antibiotics are deemed necessary. The preoperative intravenous use of corticosteroids is a significant element in preventing edema after surgery. In order to prevent arthrofibrosis, hemarthrosis, and train the muscles of mastication to stretch after TMJ arthroscopic procedures, it is frequently essential to start mandibular motion and opening. This capacity to achieve the objective of enhanced mandibular functioning is hampered by edema. As a result, it is advised to administer corticosteroids in tapered doses after surgery.
In patients with habitual TMJ luxation, arthroscopic electrocautery of the TMJ is a relatively straightforward procedure with positive results. Intermaxillary fixation, bone grafting, and foreign material implantation into the joint are not necessary. It is believed that electrocautery impacts the retrodiscal tissues, causing an unintentional stiffening of the loose bilaminar zone tissues. Anterior disc displacement (ADD) has been related to pain in ID of the TMJ Lin et al. 2012.[11] The disc is not innervated, but it is attached to the articular capsule with highly innervated tissue. Lateral and medial rigid insertions give fibrocartilage coverage to the condyle head Alomar et al., 2007.[12] When ADD is confirmed, the collapse of the posterolateral recess occurs, leading to the elongated retrodiscal tissue being subjected to trauma between the articular surfaces. Arthroscopic retention of the recaptured disc represents a minimally invasive technique that essentially alters established anatomical disorders, specifically addressing the elongation of retrodiscal tissue, its trauma during joint loading, and its movement between the articular surfaces. The disc is affixed to the posterolateral aspect of the condylar head using resorbable pins, allowing the retrodiscal tissue to relax and restore the previously collapsed lateral recess.
Discectomy stands as the oldest and frequently utilized procedure for addressing painful TMJs with ID. The application of a Holmium YAG laser in arthroscopic discectomy yielded a comprehensive success rate of 93.33%.[13] Numerous prospective long-term investigations have demonstrated the effectiveness of discectomy in relieving pain and enhancing mandibular function among individuals experiencing ID of the TMJ.[14–16]
Performing arthroscopic discectomy results in minimal impact on the surrounding tissues, minimizing the formation of scar tissue and providing improved visibility for assessing the integrity of the vascular and lymphatic systems. Complications following discectomy are infrequent, with literature indicating a 1% occurrence linked to temporary paresis of the frontal or zygomatic branches of the facial nerve and less than 0.1% associated with infections.[17]
The patient must be instructed individually regarding postoperative training, depending on the type of procedure performed. In patients with chronic locking who have undergone lysis and lavage, more intensive training should be recommended, and in those who have had disk repositioning and restriction procedures, training should be introduced gradually. The length of the follow-up period should be at least one year.
CONCLUSION
Temporomandibular disorders (TMDs) are currently diagnosable and manageable through arthroscopy within the field of oral and maxillofacial surgery. This method provides an added advantage of performing simultaneous biopsies in the target area with minor and infrequent complications, ensuring a high level of accuracy in TMD diagnosis. The growing use of surgical lasers on the TMJ has further enhanced the viability of arthroscopic surgery, offering both immediate favorable outcomes and economic benefits. Ultimately, arthroscopy presents new avenues for research, allowing for a clearer understanding and in-depth exploration of the etiopathogenesis of TMDs.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent is not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Arthroscopy of the temporomandibular joint: Technique and operative images. Atlas Oral Maxillofac Surg Clin North Am. 2003;11:129-44.
- [CrossRef] [PubMed] [Google Scholar]
- Operative maxillofacial surgery. In: Langdon JD, Patel MF, eds. Chapter 3: Temporomandibular joint arthroscopy and endoscopy. London: Chapman & Hall; 1998. p. :25-39.
- [Google Scholar]
- Arthroscopy of the temporomandibular joint. J Jpn Stomatol Soc. 1975;42:207-13. [in Japanese]
- [Google Scholar]
- Clinical application of arthroscopy in the temporomandibular joint disease. Bull Tokyo Med Dent Univ. 1980;27:141-50.
- [PubMed] [Google Scholar]
- Arthroscopic surgery for hypermobility and recurrent mandibular dislocation. Oral Maxillofac Surg Clin North Am. 1989;1:153-6.
- [Google Scholar]
- Newly designed needle scope system for arthroscopic surgery by double-channel sheath method. Jjpn Soc TMJ. 1989;1:209-16. [in Japanese]
- [PubMed] [Google Scholar]
- Arthroscopy - TMJ internal derangement disorders-diagnostic and surgical. Lambert Academic Publishing; 2018. p. :1-65. (ISBN 978-613-9-58360-7)
- TMJ arthroscopy: A review article & recent advances. The Traumaxilla. 2022;1:63-70.
- [Google Scholar]
- Diagnostic and surgical arthroscopy of the temporomandibular joint: Clinical experience with 137 procedures over a 2-year period. J Craniomandib Disord Facial Oral Pain. 1987;1:202.
- [PubMed] [Google Scholar]
- Current thinking in temporomandibular joint management. Br J Oral Maxillofac Surg. 2009;47:91-4.
- [CrossRef] [PubMed] [Google Scholar]
- The use of pseudo-dynamic magnetic resonance imaging for evaluating the relationship between temporomandibular joint anterior disc displacement and joint pain. Int J Oral Maxillofac Surg. 2012;41:1501-4.
- [CrossRef] [PubMed] [Google Scholar]
- Anatomy of the temporomandibular joint. Semin Ultrasound CT MR. 2007;28:170-83.
- [CrossRef] [PubMed] [Google Scholar]
- Long-term evaluation of arthroscopic discectomy of the temporomandibular joint using the holmium YAG laser. J Oral Maxillofac Surg. 2001;59:1018-23.
- [CrossRef] [PubMed] [Google Scholar]
- Temporomandibular joint diskectomy: No positive effect of temporary silicone implant in a 5-year follow-up. Oral Surg Oral Med Oral Pathol. 1992;74:259.
- [CrossRef] [PubMed] [Google Scholar]
- Diskectomy in treatment of internal derangement of the temporomandibular joint. Follow-up at 1, 3, and 5 years. Oral Surg Oral Med Oral Pathol. 1993;76:266.
- [CrossRef] [PubMed] [Google Scholar]
- Diskectomy in temporomandibular joints with internal derangement: A follow-up study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;83:314.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic management of internal derangements of the temporomandibular joint. Oral Maxillofac Surg Clin North Am. 1994;6:259.
- [Google Scholar]







