Translate this page into:
Tessier 7– Facial Cleft with Macrostomia: A Rare Case Report

*Corresponding author: Priyankar Singh, Unit of Craniomaxillofacial Surgery, Post Graduate Institute of Dental Education and Research (PGIDER), Indira Gandhi Institute of Medical Sciences, Sheikhpura, Patna, India. spriyankar@yahoo.co.in
-
Received: ,
Accepted: ,
How to cite this article: Anwar E, Akhtar M, Singh P, Singh N, Mishra N, Sharma AK. Tessier 7– Facial Cleft with Macrostomia: A Rare Case Report. Dent J Indira Gandhi Int Med Sci. 2024;3:68–70. doi: 10.25259/DJIGIMS_4_2024
Abstract
The literature rarely reports unilateral Tessier no. 7 clefts. Tessier no. 7 craniofacial clefts, also called temporozygomatic or transverse facial clefts, are the most laterally located type of craniofacial clefts. History of the patient, clinical presentation, and Computed tomography (CT)scan were considered as the diagnostic criteria. The hasty analysis and surgical correction of craniofacial defect is essential because it may disturb the facial development of the patient.
Keywords
Tessier 7 cleft
Z-plasty
Orbicularis oris muscles
INTRODUCTION
Tessier 7 cleft is a distinctive anomaly within the Tessier craniofacial cleft classification system, which delineates congenital facial clefts [Figure 1]. The actual number of incidences of Tessier no. 7 cleft is unidentified.[1, 2] Poswillo stated that in the early stage of embryogenesis, when there is an interruption of the stapedial artery, this cleft occurs.[3] Lateral facial muscular diastasis, macrostomia, and bony abnormalities in zygoma as well as maxilla are present in Tessier no. 7 cleft that is a lateral cleft.[4]
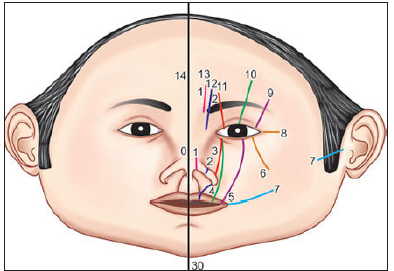
- Tessier craniofacial cleft classification, Oral Nasal: Clefts 0-3, Oral-Ocular: Clefts 4-6, Lateral Facial: Cleft 7-9, Cranial: 10-14.
Unilateral facial clefts are six times more prevalent compared to bilateral facial clefts. The defects are symmetrical in the case of bilateral facial clefts though uncommonly asymmetry is noted.[5] This classification underscores the complexity of craniofacial malformations, requiring a detailed understanding for accurate diagnosis and appropriate management. Exploring the features and nuances of Tessier 7 cleft is pivotal in the comprehensive study of craniofacial abnormalities and informs the multidisciplinary approach essential for the care of affected individuals. We hereby report a rare Tessier 7 cleft operated at the comprehensive cleft care center of our institute and recommend early surgical intervention as reported by other studies.[6]
CASE REPORT
This case is of an 8-month-old baby boy with Tessier 7 cleft on the left side, involving a unilateral cleft on the left side of his mouth. This typical case emphasizes the worth of a multidisciplinary approach, incorporating clinical examination, imaging studies, feeding assessment, psychological evaluation, and preoperative assessment.
The baby boy was brought in by concerned parents, who noticed a gap on the left side of his mouth since birth. Feeding difficulties prompted their visit, seeking guidance on the best way to care for their child. On clinical examination, a unilateral cleft on the left side, impacting the upper lip and extending into the maxillary region, was noticed [Figure 2]. During functional assessment, the child exhibited challenges with feeding, warranting further investigation. Imaging studies like plain x-rays were performed to assess the bony structures of the maxilla, providing insights into potential skeletal anomalies associated with the cleft. A preoperative evaluation,including blood tests, chest x-ray, and 2-D echo was performed to ensure the child’s general health and readiness for potential surgical intervention. During the surgical procedure initially, the dimple of the philtrum was marked. Measurement was done between the philtrum and the oral commissure of the normal side and then on the cleft side. Hence, on the upper lip of the cleft side, the commissural point was made, and the opposite point of this commissure point was marked on the lower lip. Horizontal incision was made between the commissure point and the termination of the cleft on the skin and vermillion border. The vermilion borders on the upper lip and lower lip were dissected,and for creating the inside mucosa of the commissure, the suturing of orbicularis oris muscles was performed. The congenitally disturbed orbicularis oris muscles were exposed. Intentional overlapping of the orbicularis oris muscles on both sides was done and sutured for making the continuity of oral sphincter. A small Z-plasty was carried out on the skin near the oral commissure, and the resulting gap was primarily stitched [Figure 3]. To restrict mouth movement, a liquid diet was maintained for the first five days after the operation. On the 10th day, the skin stitches were taken out, and there were no observed complications during the recovery period.

- Preoperative photographs.

- Postoperative photographs.
DISCUSSION
The transverse facial cleft, known as congenital macrosomia or Tessier cleft no. 7, is a rare birth defect. Treacher Collins syndrome exhibits a combination of Tessier numbers 6-7-8. However, tessier 7 cleft is specifically associated with hemifacial microsomia and represents the most lateral facial cleft, affecting both facial and cranial areas. Symptoms include macrostomia, preauricular skin tag, microtia, the temporomandibular joint absence, zygomatic arch, eyelids, accessory maxilla, polydactyly, and potential cardiac anomalies. The failure of fusing the mandible and maxilla processes of the first branchial arch attributes its origin. In addition, physical restricting forces like amniotic bands are also considered as a culprit, supported by experimental studies by Stelnicki et al.[7,8]
The transverse facial clefts are mostly male predilected, which tend to be on the left side. The clinical features of Tessier 7 cleft includes distinct manifestations in the affected facial region. Upper Lip Abnormalities: Tessier 7 cleft frequently results in a cleft of the upper lip, which can extend from a minor notch to complete separation. The cleft extends into the maxilla, affecting the bony structures of the upper jaw. This can cause asymmetry and deformities in the midface. Tessier 7 cleft can affect the development of teeth in the affected area, resulting in dental malformations and misalignments. The cleft may extend into the nasal structures, changing the shape and function of the nose. As a result of the structural abnormalities in the oral and nasal regions, people with Tessier 7 cleft may have difficulty speaking and feeding. Facial esthetics are severely impacted, necessitating comprehensive interventions that address both functional and cosmetic aspects. Various classification systems, including those by the American Association of Cleft Palate Rehabilitation, Karfik, Boo-Chia, Demeyer, and Van der Meulen,[1,2,4,9] exist, but Tessier classification, established through clinical analysis, is widely accepted. Hypoplasia is observed in the zygoma, temporal bone, maxilla, mandible, parotid gland, parotid duct, and innervation areas of the fifth and seventh cranial nerves, as well as the palate and tongue.[10] Numerous surgical techniques have been described,although the goal rectifications are the symmetrical shape of lip commissure, reestablishing oral sphincter, and quality of scar formed post z-plasty. This case yielded a satisfactory functional and esthetic result when visited for follow-up.
CONCLUSION
It is important to diagnose all Tessier cleft precisely and early surgical treatment is the prime goal.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
Arbind Kumar Sharma, Nimmi Singh, Navin Mishra, Priyankar Singh are on the editorial board of the Journal.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Rare craniofacial clefts. In: McCarthy JG, ed. Plastic surgery (1st edition). Philadelphia: WB Saunders Company; 1990. p. :2922-73.
- [Google Scholar]
- Craniofacial clefts. In: Aston SJ, Beasley RW, Thorne HC, eds. Grabb and Smith’s surgery (1st edition). New York: Lippincott-Raven; 1977. p. :349-63.
- [Google Scholar]
- The pathogenesis of the first and second branchial arch syndrome. Oral Surg Oral Med Oral Pathol. 1973;35:302-28.
- [CrossRef] [PubMed] [Google Scholar]
- Anatomical classification of facial, craniofacial and latero-facial clefts. J Maxillofac Surg. 1976;4:69-92.
- [CrossRef] [PubMed] [Google Scholar]
- Tessier’s cleft no. 7 with asymmetrical involvement. Plast Reconstr Surg. 1995;96:224-5.
- [Google Scholar]
- Craniofacial microsomia. In: McCarthy JG, ed. Plastic surgery (1st edition). Philadelphia: WB Saunders Company; 1990. p. :3054-100.
- [Google Scholar]
- A new in utero model for lateral facial clefts. J Craniofac Surgery. 1997;8:460-5.
- [CrossRef] [PubMed] [Google Scholar]
- The in-utero repair of tessier number 7 lateral facial clefts created by amniotic band-like compression. J Craniofac Surg. 1998;9:557-62.
- [CrossRef] [PubMed] [Google Scholar]
- A morphogenetic classification of craniofacial malformations. Plast Reconstr Surg. 1983;71:560-72.
- [CrossRef] [PubMed] [Google Scholar]
- Craniofacial anomalies and principles of their correction. In: Georgiade GS, Riefkohi R, Levin LS, eds. Plastic, maxillofacial and reconstructive surgery (3rd edition). Baltimore: Williams & Wilkins; 1997. p. :273-90.
- [Google Scholar]







