Translate this page into:
Precision Prosthodontic Rehabilitation of Flabby Ridge with a Modified Window Technique: Case Report

*Corresponding author: Arpit Sikri, Department of Prosthodontics, Crown & Bridge, and Oral Implantology, Bhojia Dental College & Hospital, Budh Teh.Baddi, Distt. Solan, Himachal Pradesh, India. arpitsikri@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sikri A, Kalra V, Sikri J, Jassal P, Yamika. Precision Prosthodontic Rehabilitation of Flabby Ridge with a Modified Window Technique: Case Report. Dent J Indira Gandhi Int Med Sci. 2024;3:51–64. doi: 10.25259/DJIGIMS_1_2024
Abstract
Flabby ridge, also known as a soft (mobile), movable, or displaceable ridge, presents a common clinical challenge in dental practice. It primarily affects the alveolar ridges of the upper (maxillary) or lower (mandibular) arches. The anterior region of the maxilla is especially susceptible in edentulous patients. The flabby ridge lacks the firmness and stability required, leading dentures to become loose and unstable. Consequently, this instability can result in discomfort, speech and eating difficulties, and reduced quality of life for denture wearers. The flabby ridge often does not provide the necessary contour and resilience needed to establish an effective seal and maintain suction between the denture base and the underlying tissues. This compromises denture retention, making them susceptible to dislodgement during typical oral functions. Therefore, rehabilitating a completely edentulous patient with flabby tissue presents a formidable challenge for prosthodontists, as it undermines the retention, stability and support of complete dentures. Methods for managing flabby ridges encompass surgical removal, ridge augmentation, specialized impression techniques, balanced distribution of occlusal loads and implant therapy. Various impression techniques have been proposed to address the complexities of such cases. By carefully applying the principles of complete denture construction, a palliative treatment approach can be achieved. Special impressions often employ the window technique to capture a static impression of the flabby area, which introduces its own set of challenges.
This innovative case report introduces a modified window technique that incorporates precise record transfer of the flabby ridge using tissue (blotting) paper. Specifically designed for the anterior mandibular flabby ridge, the technique employs a custom tray with a window positioned over the flabby tissues. A mucostatic impression material is utilized to minimize pressure on the flabby tissue, thereby reducing potential tissue distortion during the impression process. The procedure is executed in two steps: first, stable structures are recorded, followed by capturing the mobile tissues using light-body polyvinyl siloxane (PVS) elastomeric impression material within the window area. This method ensures an accurate record of the denture-supporting structures while maintaining the contour and details of the flabby tissues without displacement. Importantly, the technique is crafted for straightforward implementation by general dental practitioners within a primary dental care setting.
Keywords
Complete denture
Edentulous
Fibrous tissue
Flabby tissue
Hypermobile tissue
Impression technique
Modified window technique
Monophase polyvinyl siloxane impression material
Mucostatic
INTRODUCTION
The goal of complete denture prosthodontics is to enhance appearance, comfort and functionality by replacing lost dental and underlying bony tissues with stable prostheses. Ideally, the residual ridge should be covered with a layer of masticatory mucosa, typically 1.5–2 mm thick. This ensures proper soft tissue support for the denture, a point emphasized by Desjardins and Tolman in 1974.[1]
The effectiveness of a complete denture largely relies on its retention, stability and support during function. A precise impression for a complete denture should encompass all functional denture-bearing, relief and limiting areas, striving for optimal retention, stability and support. Challenges emerge when the areas intended to support the denture prove suboptimal, showcasing soft or movable areas, often referred to as ‘displaceable’ or ‘flabby ridges,’ within the denture’s base.[2]
The flabby ridge, also known as a mobile or displaceable ridge, is a common challenge in dentistry. It is characterized by an excess of soft tissue in edentulous areas, particularly on the superficial aspect of the alveolar ridge. This surplus tissue, resulting from the replacement of bone with fibrous connective tissue, compromises the denture’s retention, stability and support. Often referred to as a fibrous or movable ridge, this condition typically arises when an overgrowth of soft tissue replaces the alveolar bone.[3] It is especially prevalent in the upper (maxillary) anterior region among individuals who ‘ve worn dentures for extended periods. The occurrence of flabby ridges varies between the upper and lower jaws, with a prevalence of 24% in the edentulous upper (maxillary) jaw compared to 5% in the lower (mandibular) jaw.[4]
The direct causes of bone resorption and tissue atrophy in the mouth are not fully understood. However, several factors contribute to these changes, particularly among denture wearers. Chronic irritation from ill-fitting dentures, mismatched occlusion and traumatic fitting surfaces are significant culprits. Excessive pressure on the anterior part of the ridge, often resulting from specific chewing habits or inconsistent denture materials, can induce stress and subsequent complications. Such pressure can accelerate the resorption of the ridge’s anterior portion, leading to a narrow, knife-edge shape.[5] Prolonged denture use may also culminate in flabby tissue, where thickened mucosa replaces bone. This condition frequently stems from poorly fitting dentures that cause persistent trauma.[6] In some instances, natural mandibular teeth can exacerbate the issue in the maxillary region, resulting in bone loss and the proliferation of fibrous tissue. These flabby ridges are particularly prevalent when a denture ridge interfaces with natural teeth, a phenomenon termed the Combination Syndrome when observed in the anterior maxillary region.[7] Factors such as wearing dentures overnight or natural teeth encroaching too far onto an edentulous ridge further exacerbate the issue. The precise etiology of these conditions is multifaceted and not entirely elucidated, suggesting a blend of physiological and clinical factors.
Histologically, when examining flabby or fibrous tissue associated with the oral mucosa, one typically observes mucosal hyperplasia, which refers to an abnormal increase in the number of cells in the mucosal layer. This hyperplasia can arise as a response to chronic irritation or other stimuli, leading to an overgrowth of the mucosal layer. Additionally, the tissue often contains a mixture of fibrous components, with fibers that can be either loosely arranged or more densely packed, providing support and structure to the surrounding areas. Moreover, the presence of dense collagen connective tissue is notable, as collagen serves as the main structural protein in the body, offering strength and resilience to tissues. Specifically, in the context of flabby or fibrous tissue, there is an accumulation of dense collagen fibers, contributing to the tissue’s fibrous nature. In essence, the histological composition of flabby or fibrous tissue reflects a combination of cellular hyperplasia and alterations in the connective tissue matrix.[8] Recognizing and understanding these histological features is crucial for both diagnosis and treatment planning.
Managing flabby ridges in denture fabrication presents numerous challenges and therapeutic options. Surgical interventions, such as using scalpels or sclerosing agents, can precede denture creation, but they may increase the denture’s bulk and pose a higher risk of injuries.[9] While ridge augmentation surgery exists, it can compromise both denture stability and the soft tissue’s stress-absorbing capacity. An alternative approach involves implant-retained prostheses, where dental implants are utilized to bolster stability. This process encompasses bone augmentation, implant insertion, and the integration of overdentures. On the other hand, some individuals opt for non-surgical conventional prosthodontics, relying on advanced impression techniques to achieve an ideal fit without resorting to surgery. Conventional prosthodontic methods, which include meticulous impression techniques and occlusal load adjustments, are widely adopted. Although the impression phase is crucial, it can inadvertently reshape flabby tissues, affecting both function and aesthetics. As a result, a diverse range of strategies, spanning both surgical and prosthodontic realms, have been developed to address flabby ridges.[10] When fabricating dentures on such complex foundations, the chosen approach often depends on factors like the patient’s health, the extent of ridge flabbiness, financial considerations, and the prosthodontist’s expertise. For instance, surgically reducing the tissue might be paired with increasing the denture’s base thickness, though this could also increase its weight. Each method has its own set of advantages and limitations, highlighting the importance of tailoring solutions in denture fabrication. It is essential to weigh the pros and cons of each procedure carefully.
This case report introduces a novel technique for capturing precise records of the flabby ridge in the anterior mandibular area, termed the modified window technique. This approach employs a custom tray equipped with a window designed to target flabby tissues, ensuring minimal pressure and reduced distortion. The procedure is bifurcated into two steps: initially recording stable structures, followed by capturing mobile tissues using a specialized material within the window. The primary objective of this technique is to precisely represent denture-supporting structures while maintaining the natural contour of the flabby tissues. Importantly, its design facilitates straightforward adoption by general dental practitioners in primary care settings.
CASE REPORT
A 45-year-old woman with no remaining natural teeth presented to the Department of Prosthodontics, Crown & Bridge, and Oral Implantology. She primarily complained about poorly fitting upper and lower dentures, which had been causing her discomfort and hindering her ability to eat for the past three years. The patient previously had teeth removed due to dental caries.
The patient’s overall health was described as average. Regarding oral care practices, she regularly rinsed her mouth twice daily. Furthermore, there were no other notable habits or issues related to her oral or overall health. The patient had a relatively unremarkable medical history. However, her dental history indicated that she had been using a complete denture for the last 15 years [Figures 1a and 1b].

- Previous removable dental prostheses of the patient (Intaglio surface).

- Previous removable dental prostheses of the patient (Occlusal surface).
The patient’s socio-psychological status indicated that she was married and had two children. In terms of her educational background, she had completed upper secondary education, equivalent to a 10+2 level. Furthermore, the patient exhibited a philosophical disposition (attitude).
During the extra-oral examination, several observations were noted. The patient’s facial form was square-tapering, and her profile was described as convex, with a prognathic maxilla and a retrognathic mandible. Interestingly, her facial symmetry appeared to be symmetrically asymmetrical. The facial height was within the normal range, and her facial muscle tone was also considered normal. The individual had brown eyes and a medium complexion. Her lips were thin, and the overall length of her face was average. Upon examination of the temporomandibular joint (TMJ), everything appeared normal. Additionally, the lymph nodes were found to be non-palpable and non-tender.
Intraoral examination revealed a flabby mandibular anterior edentulous ridge and a conventional maxillary edentulous ridge [Figures 2a and 2b]. The flabby ridge was identified by applying pressure to the tissue using a T-burnisher and the back of an intraoral mirror. Upon application of pressure, tissue blanching was observed [Figure 3].

- Edentulous maxillary residual alveolar ridge.

- Edentulous mandibular residual alveolar ridge.

- Flabby anterior mandibular edentulous ridge – pressure application using the back of the intraoral mirror.
Upon evaluating the residual ridges, several observations were made. The arch form for the maxilla was U-shaped, while the mandible was V-shaped. The residual ridge form in the maxillary region was high and well-rounded, whereas in the mandibular region, it appeared as a knife edge. The interarch distance was considered adequate, and the primary undercut location was in the mandibular anterior region. Importantly, no bony irregularities were detected. Regarding the mucosa, both the lip mucosa and cheek mucosa appeared normal. Within the floor of the mouth, the lingual frenum and plica were normal, and the retromylohyoid fossa was classified as Type-1. The tongue exhibited normal mucosa and size, along with a typical gag reflex. In terms of the palate, the incisive papilla, rugae and mucosa all appeared normal. The palatal vault was U-shaped, and the junction of the hard and soft palate was categorized as Class 1. The posterior palatal seal (PPS) area was compressible. Within the vestibule, the maxillary region was deep both labially and buccally, whereas the mandibular region was shallow in the same dimensions. Frenal attachments appeared normal, and the observed saliva was mixed with a normal quantity.
The patient was presented with various treatment options, including surgical procedures, implant-supported fixed and removable prostheses, and conventional prosthodontic rehabilitation. After discussing these options with the patient and considering his reluctance towards surgical treatments and budgetary (financial) constraints, the decision was made to proceed with fabricating removable complete dentures as the preferred method of prosthodontic rehabilitation. A comprehensive treatment plan was devised to fabricate the removable complete dentures. This plan integrated a specialized impression technique tailored for the flabby tissue of the edentulous mandibular anterior ridge and a conventional impression technique for the edentulous maxillary ridge. The objective was to capture the flabby tissue accurately, preventing displacement, while ensuring an optimal fit, support and stability throughout the denture base. This approach aimed to minimize denture movement during use. Before initiating the treatment, the patient gave an informed consent, including permission for potential publication of the case in future literature.
PROCEDURE
The initial stages of the complete denture fabrication process were as follows:
-
Preliminary impressions: Impressions of both the upper (maxillary) and lower (mandibular) jaws were made using a medium fusing impression compound (Hiflex Impression Compound, Prevest DenPro Limited, Jammu, India). Subsequently, the impression compound was gently scraped away, and a subsequent impression was made with a thin mix of irreversible hydrocolloid using the corrective primary impression technique (Zelgan 2002, Dentsply India Pvt. Ltd., Haryana, India) [Figures 4a and 4b]. The areas with flabby tissues were distinctly marked using an indelible pencil.
 Figure 4a:
Figure 4a:- Corrective maxillary primary impression.
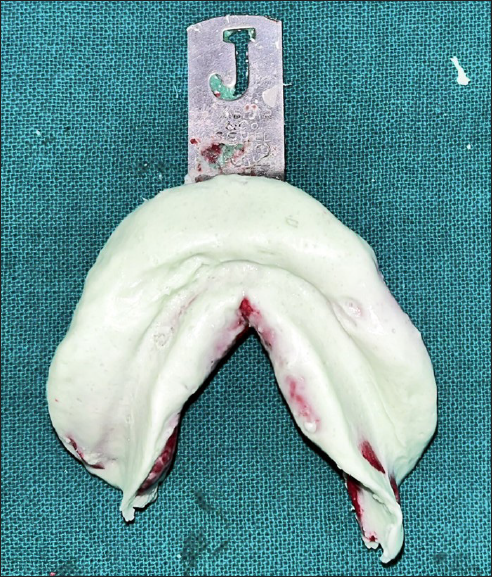 Figure 4b:
Figure 4b:- Corrective mandibular primary impression.
Primary cast preparation: The primary impressions were beaded and boxed using beading and boxing wax, respectively (MAARC Dental, Maharashtra, India). A primary cast was then derived using type II dental plaster (GypRock plaster, Rajkot, Gujarat, India) [Figures 5a and 5b]. The outline of the flabby ridge area from the impression was accurately transferred onto this preliminary cast.
 Figure 5a:
Figure 5a:- Preliminary maxillary cast.
 Figure 5b:
Figure 5b:- Preliminary mandibular cast.
-
Spacer application: The thickness of the wax spacer was confirmed using a Dental Gauge Wax Caliper (Caliper Iwanson Wax, GDC Fine Crafted Dental Pvt. Ltd., Hoshiarpur, India) [Figure 6]. Subsequently, a double-thickness wax spacer (MAARC Dental, Maharashtra, India) [Figure 7] was carefully positioned over the flabby tissue region to ensure sufficient relief.
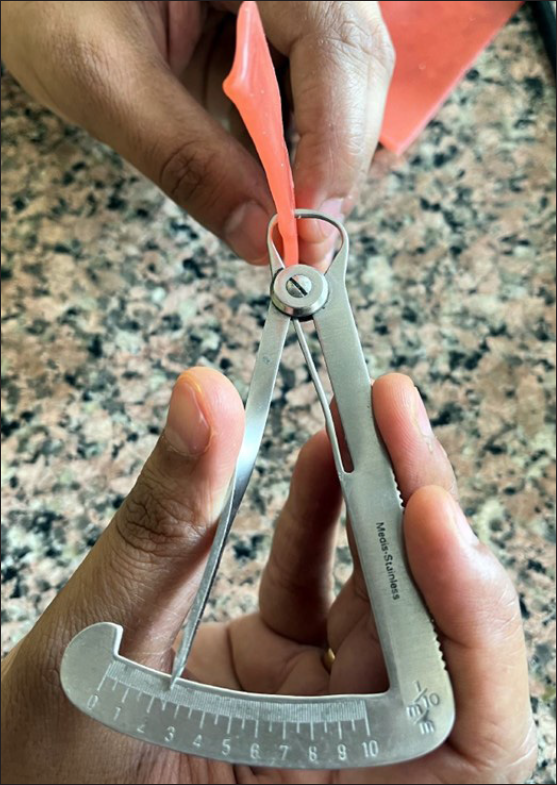 Figure 6:
Figure 6:- Spacer thickness verification using Dental Gauge Wax Caliper.
 Figure 7:
Figure 7:- Double-thickness wax spacer adaptation (mandibular).
-
Custom tray fabrication: The custom trays were fabricated using autopolymerizing acrylic resin (DPI RR Cold Cure, Dental Products of India, Mumbai, India) [Figure 8].
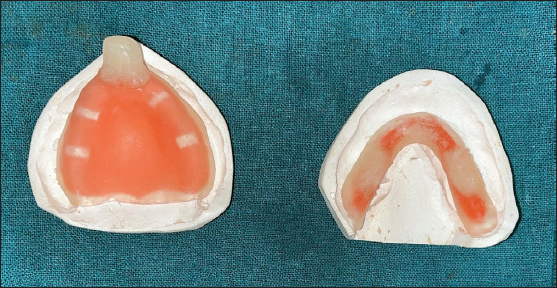 Figure 8:
Figure 8:- Custom trays (maxillary and mandibular).
-
Border molding: The process of border molding was carried out using a low-fusing green stick compound (Pinnacle Tracing Sticks, Dental Products of India, Mumbai, India) [Figures 9a and 9b]. Once the border molding was finalized, the wax spacers on the custom trays were removed [Figure 10].
 Figure 9a:
Figure 9a:- Border molding (maxillary).
 Figure 9b:
Figure 9b:- Border molding (mandibular).
 Figure 10:
Figure 10:- Wax spacer removal after completion of border molding (mandibular).
-
Final impression: The definitive impressions were then taken: the edentulous mandibular ridge was captured using monophase polyvinyl siloxane (PVS) elastomeric impression material (Aquasil Ultra Monophase, Dentsply India Pvt. Ltd., Mumbai, India) [Figure 11a], while the edentulous maxillary ridge employed the conventional zinc oxide eugenol wash impression method (DPI Impression Paste, Dental Products of India, Mumbai, India) [Figure 11b]. After obtaining the final impression using monophase impression material, a tissue (blotting) paper was placed over the mandibular anterior region of the impression surface [Figure 12]. The area of flabby tissue was then marked using an indelible pencil, and the outline of the flabby ridge was transferred from the impression onto the blotting paper [Figure 13]. Based on this outline, a window was created to reduce hydraulic pressure during the impression process, thereby minimizing tissue distortion [Figures 14a and 14b]. Once the window was successfully established, the final impression of the flabby ridge was recorded using low-viscosity PVS elastomeric impression material (Aquasil Ultra LV Light Body, Dentsply India Pvt. Ltd., Mumbai, India), applied with the assistance of a syringe [Figures 15a and 15b]. The final impression using Modified Window Technique is illustrated in Figure 16.
 Figure 11a:
Figure 11a:- Final impression (mandibular) using monophase polyvinyl siloxane elastomeric impression material.
 Figure 11b:
Figure 11b:- Final impression (maxillary) using zinc oxide eugenol impression paste.
 Figure 12:
Figure 12:- Placement of tissue (blotting) paper over the mandibular anterior region of the impression surface.
 Figure 13:
Figure 13:- Outline of the flabby ridge transferred from the impression onto the blotting paper.
 Figure 14a:
Figure 14a:- Window preparation in the custom tray (Outside the patient’s mouth).
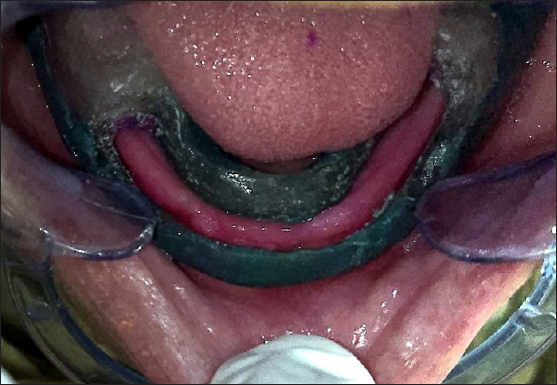 Figure 14b:
Figure 14b:- Window preparation in the custom tray (Evaluation of the tray inside the patient’s mouth).
 Figure 15a:
Figure 15a:- Final impression of the flabby ridge using low-viscosity polyvinyl siloxane elastomeric impression material with a syringe.
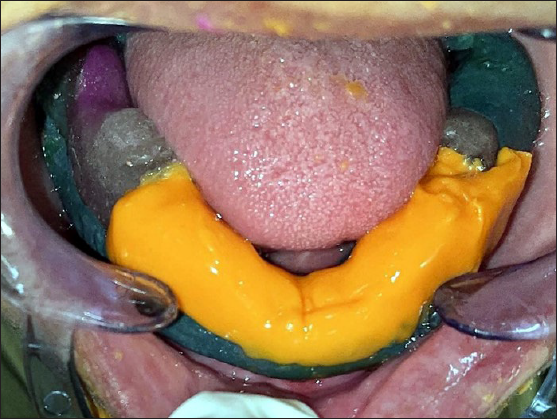 Figure 15b:
Figure 15b:- Final impression of the flabby ridge (Evaluation in patient’s mouth).
 Figure 16:
Figure 16:- Final impression using Modified Window Technique.
-
Master (Definitive) cast preparation: The final impressions were beaded and boxed using beading and boxing wax, respectively (MAARC Dental, Maharashtra, India) to facilitate the creation of well-defined master casts. The master casts were poured using type III dental stone (GypRock stone, Rajkot, Gujarat, India) [Figure 17].
 Figure 17:
Figure 17:- Master (Definitive) casts (maxillary and mandibular).
Denture base and occlusal rim fabrication: Temporary denture bases along with occlusal rims were constructed on the definitive casts.
Facebow transfer: The orientation jaw relation was captured using a facebow (HanauTM Springbow, Whip Mix, Kentucky, USA) and then transferred to the semi-adjustable articulator (HanauTM Wide-Vue, Whip Mix, Kentucky, USA).
-
Centric jaw relations: Subsequent adjustments were made following the facebow transfer. After recording the centric relation with the Nick and Notch method [Figure 18], the casts were articulated in the semi-adjustable articulator. After occlusal registration, teeth selection was completed. The arrangement of artificial teeth was then adjusted based on established principles.
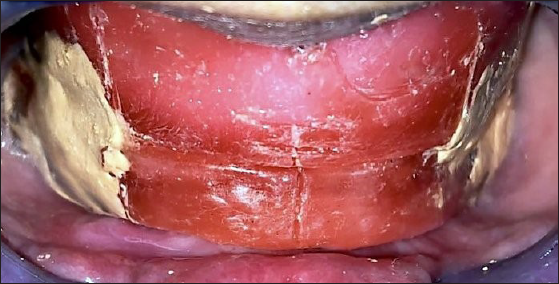 Figure 18:
Figure 18:- Jaw relation record using Nick and Notch method.
-
Trial and sealing: An intra-oral assessment of the waxed-up trial denture ensured its function, fit and esthetics [Figure 19]. Following this, the trial denture base was sealed to the definitive casts and separated from the articulator.
 Figure 19:
Figure 19:- Waxed-up try in.
Flasking: Both the maxillary and mandibular arches underwent the flasking procedure.
Processing: After dewaxing, a tin foil substitute (DPI Heat Cure Cold Mould Seal, Dental Products of India, Mumbai, India) was applied. The dentures were then packed, pressed and processed traditionally (DPI Heat Cure, Dental Products of India, Mumbai, India).
Cleaning: The finished dentures were cleaned using an ultrasonic cleaner.
-
Final evaluation: The dentures underwent finishing and polishing before being tried in the patient’s mouth. Any necessary adjustments to the aesthetics or occlusion were made. Upon finalizing these adjustments, both the upper and lower removable complete dentures were delivered to the patient [Figure 20].
 Figure 20:
Figure 20:- Removable complete dentures – in patient’s mouth.
-
Post-denture insertion care: The patient received instructions on denture care and maintenance after the insertion of the dentures. Follow-up evaluations were conducted at 24 hours, 1 week and 1 month. Ultimately, the patient expressed satisfaction with the aesthetics, speech clarity and functionality of the newly fitted complete dentures [Figure 21].
 Figure 21:
Figure 21:- Patient follow-up.
DISCUSSION
The primary objectives of complete denture rehabilitation focus on restoring function, improving appearance, ensuring comfort and maintaining the patient’s overall oral health. The success of a complete denture hinges on its support and retention. To achieve optimal stability, it is crucial that a precise master impression captures the entire functional area where the denture will rest. Such precision in the impression is fundamental for ensuring both stability and retention of the prosthesis.[11] In traditional settings, attaining this level of accuracy is typically feasible and dependable. However, complications can arise when the supportive areas are not ideal. The forces generated during chewing can dislodge these areas, causing the denture to fit inadequately and jeopardizing its seal. If these mobile areas are not managed meticulously during the impression process, they can distort over time. Ideally, the masticatory mucosa should have a thickness ranging between 1.5 and 2 mm; any deviation from this can impact the denture’s fit. A significant obstacle in denture fabrication is addressing unstable ridges that tend to shift unpredictably. Such ridges compromise the denture’s ability to remain secure, leading to decreased retention. Ridges that exhibit excessive movement, surpassing 2 mm, pose substantial challenges to the denture’s support and stability, often requiring specialized impression techniques for effective resolution.[12]
In certain atypical scenarios, such as with a flabby ridge, the residual portion of the alveolar bone or the edentulous ridge can undergo significant changes. Instead of retaining its firmness, it may transform into hyperplastic, fibrous or excessively mobile soft tissue, which lacks adequate bone support. This hypermobile or flabby tissue is commonly observed in the edentulous maxillary anterior region or can overlay a knife-edge atrophic mandibular ridge. Several factors contribute to the development of this fibrous tissue. A prominent factor is the excessive occlusal loading on the edentulous maxillary residual alveolar ridge, often resulting from unstable occlusal relationships or unconventional teeth arrangements. This heightened pressure leads to the resorption of the residual alveolar bone, which is then replaced by the softer, flabby tissue. Such tissue provides insufficient support for complete dentures. Moreover, masticatory forces can dislodge this flabby tissue, causing shifts in the denture’s position and compromising both its fit and peripheral seal.[13]
In a clinical examination for flabby ridges, it is essential to begin with a comprehensive evaluation of the alveolar ridge and the overlying soft tissue to gain a detailed understanding of the tissue anatomy, which is crucial for accurate diagnosis and treatment planning. The use of a ball burnisher can be particularly useful, as gentle pressure applied with this tool can cause flabby tissue to blanch or turn pale, distinguishing it from firmer tissues. Furthermore, special attention should be given to edentulous areas, observing any irregularities, depressions or changes in tissue consistency, as these observations can offer insights into potential challenges during denture fabrication and fitting. A thorough history of the patient’s denture use is also paramount, including any past issues, complaints or modifications, as this information can guide the clinician in addressing specific concerns and ensuring better prosthesis outcomes. Additionally, conducting a psychological assessment to understand the patient’s psychological state and expectations is vital, given that the removable dental prostheses can significantly influence a patient’s self-esteem and quality of life. When evaluating the edentulous ridge, it is ideal for it to exhibit adequate height and width for optimal denture retention and stability. Any discrepancies or abnormalities, such as sharp bony prominences or areas of excessive soft tissue, should be carefully noted. Similarly, attention should be paid to the overall architecture and health of the mucosa, documenting any irregularities, lesions or signs of inflammation. In cases where the edentulous maxillary anterior region opposes preserved mandibular anterior teeth, or when posteriorly located flabby ridges are present, special attention is required, as these scenarios can present unique challenges. Lastly, it is crucial to take note of any patient complaints related to denture fit and function. Given the unique composition and characteristics of flabby ridges, issues such as pain, discomfort or denture looseness can arise, and addressing these concerns is paramount for patient satisfaction and treatment success. In summary, a meticulous clinical examination that combines technical evaluation with patient-centered care is pivotal in identifying, understanding, and addressing the challenges posed by flabby ridges, ensuring optimal outcomes in prosthodontic rehabilitation.[14]
Various treatment modalities exist for managing flabby tissues, encompassing both surgical and non-surgical approaches. While surgical methods like ‘surgical debulking’ aim to remove problematic tissue, they have limitations, including patient age and health concerns, potential reduction in ridge depth and decreased suitability for dental implants. Ridge augmentation with bone grafts offers another approach but has debated long-term success. Additionally, treatments such as sclerosing agents aim to firm up tissues but bring risks like allergies and discomfort. Conventional impression techniques may also result in unstable dentures, requiring frequent adjustments. Ultimately, managing flabby ridge conditions requires a thorough evaluation of treatment options to balance benefits and drawbacks for optimal patient outcomes.[15]
The prosthodontic approach emerges as a preferred treatment route, particularly emphasizing non-surgical interventions. As articulated by DeVan,[16] there is an emphasis on preserving existing structures rather than exclusively focusing on replacing lost ones. Managing challenging denture-bearing areas can indeed be daunting for prosthodontists. It becomes imperative for them to select the appropriate impression techniques and materials that can capture the flabby tissue in its natural state, ensuring optimal retention, support and stability. Beyond just impression-making, attention to detail is crucial in other facets of denture design and fabrication. Proper orientation of the occlusal plane is vital. The choice of an appropriate occlusal scheme and ensuring bilateral balanced occlusion are paramount for patient comfort and functionality. Utilizing tools like a facebow for orientation jaw relation and arranging artificial teeth on a semi-adjustable articulator can aid in achieving these objectives. Errors in the orientation of the occlusal plane or the presence of deflective occlusal contacts can compromise the stability of the complete denture. Thus, a meticulous and comprehensive prosthodontic approach is essential to ensure the success and longevity of a complete denture.[17]
Challenges arise with conventional impression techniques for patients with flabby ridges, often resulting in denture instability and reduced retention. Such issues frequently prompt patients to describe their dentures as ‘loose’. While chairside soft relines are a common remedy, they may not always address the root problem. The essence lies in employing accurate impression techniques and materials specifically designed to effectively manage flabby ridges. The literature presents a debate between mucostatic and selective pressure impression techniques, with no definitive consensus on the superior approach for ensuring stable and retentive dentures on flabby ridges.
The literature provides a plethora of impression techniques designed to address the complexities associated with flabby ridges. The optimal approach, however, remains a topic of debate, as underscored by MacEntee.[18] A widely accepted method involves recording tissues in their relaxed or resting state. This mucostatic impression technique has been advocated by numerous clinicians, including Boucher,[19] Klein and Broner,[20] Hyde et al.,[21] Devan,[16] and Zinner and Sherman.[22] Within the realm of mucostatic techniques, several variations exist. For instance, some practitioners employ double spacers, multiple relief holes or specialized window trays to accommodate flabby tissues, as highlighted by MacEntee,[18] Boucher,[19] and others.
Magnusson et al.[23] and Xie et al.[24] proposed a unique approach, utilizing two distinct impression materials within a custom tray: impression plaster for the flabby ridge and zinc oxide-eugenol for the healthier surrounding tissues. Liddelow[25] reported a similar dual-material technique. Osborne[26] employed two separate custom trays, each with a different impression material. Watt et al.[27] described a combination technique: using an impression compound in a custom tray followed by a zinc-oxide-eugenol wash impression, aiming to minimize denture base movement during mastication. Lynch and Allen[28] later revisited this approach, substituting PVS for the impression compound.
Another notable technique is the Window Impression Technique, introduced by Watson.[29] This innovative approach is specifically designed to address the challenges associated with flabby ridges in patients. The method entails creating a custom tray with a window positioned over the flabby area, facilitating the precise recording of the ridge while minimizing displacement. Following the initial impressions made with materials such as zinc oxide and eugenol, a low-viscosity impression plaster is introduced through the window to capture detailed impressions of the flabby tissues. By employing this dual-impression approach, clinicians can obtain a comprehensive representation of both the normal and flabby tissues, thereby facilitating the fabrication of a denture tailored to the patient’s unique oral anatomy. It is essential to execute each step of the technique meticulously to ensure its efficacy and achieve an optimal fit and function of the denture. In conclusion, while multiple impression techniques exist for managing flabby ridges, the selection often hinges on the clinician’s preference, the specific clinical context and the desired treatment outcomes.
According to studies by McCord and Grant[30] and Ahmed et al.,[31] the recommended procedure involves initially recording the impression inclusive of the peripheral seal. Subsequently, a window is prepared in the custom tray to capture the displaceable tissues using a low-viscosity impression material, such as impression plaster. Contrastingly, other researchers like Allen[32] and Polychronakis et al.[33] have proposed an alternative sequence. They suggest preparing a custom tray with a window before taking the final impression. This allows for accurate tracing of the functional sulcus periphery. Once the final impression is made, the displaceable tissues are then recorded in a static position through the prepared window. In both techniques, the core principle remains consistent: a mucocompressive impression for the healthy tissues is captured using materials like zinc oxide and eugenol or regular body PVS in a custom tray. After the impression material has been set, the flabby or displaceable tissues are addressed. They are painted or filled with a low-viscosity impression material, such as impression plaster, administered through the previously prepared window.
Recognizing the limitations inherent in current methods, a novel approach has recently emerged. This innovative case report introduces a modified window technique specifically designed for the precise record transfer of the edentulous mandibular anterior flabby ridge, drawing parallels with Watson’s established technique. Employing a custom tray equipped with a window, this technique utilizes mucostatic impression material to minimize tissue distortion. The procedure is executed in two sequential steps: initially capturing stable structures, followed by recording mobile tissues using light-body PVS. This groundbreaking approach ensures an accurate representation of denture-supporting structures while maintaining the natural contour and intricate details of the flabby tissue. Crucially, it is designed to be user-friendly, making it accessible for general dental practitioners in primary care settings.
The approach combines a mucocompressive/selective pressure technique for normal tissues with the use of monophase PVS elastomeric impression and low-viscosity PVS impression over the window to capture the flabby tissue in a static state. The design of the window is pivotal as it reduces pressure on the flabby tissue. Recent studies on tray designs indicate that those with windows yield the least tissue variations.[34] Including a window ensures that the low-viscosity PVS impression material is not constrained within the tray, enabling the flabby tissue to fully regain its shape while the impression material sets. The aim was to mitigate the excessive movement of soft tissues during the secondary impression phase. The overarching goal of this method was to achieve a precise registration of both the attached and unattached tissues within the denture-bearing regions. Specifically, the objective was to capture the flabby tissue in its natural, undistorted state while also accurately replicating the intricate details of the remaining denture foundation, ensuring optimal function and fit.
The conventional window technique, while pioneering in its time, has faced several challenges (issues), prompting the dental community to seek alternatives and improvements:
-
Material limitations: The reliance on conventional materials such as impression plaster, impression compound and zinc-oxide eugenol has been critiqued for being outdated. These materials might not offer the same level of accuracy, reliability or patient comfort as newer alternatives.
-
Complexity: The process of using these materials in the conventional window technique can be intricate and cumbersome. Manipulating them correctly requires skill and precision, making the procedure prone to potential inaccuracies.
-
Modern material preference and material diversity: With advancements in dental materials, polyvinyl siloxanes, often simply referred to as silicones, have become a top choice among dental professionals. These materials offer enhanced ease of use, consistency and precision, particularly in fixed prosthodontics. The contemporary dental field showcases a diverse range of materials tailored to specific requirements. Today’s polyvinyl siloxanes are available in various consistencies and application techniques, granting dental practitioners increased flexibility and adaptability.
-
Evidence gap: Despite the advancements and shifts in material preferences, there remains a notable absence of definitive evidence pinpointing the superior impression technique for complete dentures. The lack of conclusive studies mean that dental professionals often rely on experience, preference and anecdotal evidence when choosing a technique.
In essence, while strides have been made in refining impression techniques and materials in prosthodontics, continuous research and evaluation are essential to determine the most effective and reliable approaches for dental care.
The Modified Window Technique presents a refined approach to the impression process, boasting several distinct advantages:
-
Optimized design: The technique’s window design is meticulously crafted to exert minimal pressure on the flabby tissue during the impression phase. This thoughtful design ensures that the tissue is not compressed or displaced, allowing it to fully rebound as the impression material sets.
-
Enhanced visibility: The use of a clear tray design is a notable feature, granting clinicians a clear line of sight. This visibility is instrumental in observing how the impression material interacts with the flabby tissue, ensuring accurate recording of the tissue in its natural, restful state.
-
Tissue recoil: Even in situations where there might be slight pressure during the impression, the technique’s window design facilitates the flabby tissue’s ability to revert to its resting position post-impression.
-
Minimized displacement: A primary objective of the Modified Window Technique is to capture the flabby tissue with minimal displacement, aiming for an impression that represents the tissue’s natural anatomy. Concurrently, the surrounding tissues are recorded in their functional state, striking a balance between accuracy and comfort.
-
Clinical advantages: The benefits of this technique extend to the clinical realm. By ensuring improved retention, stability and support for the prosthesis, patients experience enhanced comfort and functionality. Moreover, by minimizing tissue displacement, the risk of denture instability during daily use is significantly reduced. This makes the Modified Window Technique especially valuable for patients who either prefer non-invasive procedures or have medical contraindications for surgical interventions.
-
Material considerations: The material considerations for the Window Impression Technique emphasizes the advantages of using elastomeric materials like PVS over traditional options like zinc oxide eugenol or impression plaster. Elastomeric materials offer improved properties and are easier to work with, making them preferable for impressions. Achieving uniform application of low-viscosity materials, such as PVS, is essential for obtaining accurate impressions. The use of monophase medium body PVS is particularly important in this technique, as it provides a compressive impression in areas beyond the flabby ridge. This foundational step ensures stability for subsequent applications of light body PVS, enhancing the overall precision and reliability of the impression process. Furthermore, the monophase (single-phase) impression material is a hydrophilic addition reaction silicone characterized by its elastomeric properties. It provides outstanding dimensional accuracy, high tear strength and a notable resistance to permanent deformation.
In summary, the Modified Window Technique, which integrates monophase impression material, provides a holistic solution to the challenges associated with flabby ridges. By emphasizing the importance of capturing the flabby ridge in a resting state and allowing for tissue rebound, this technique promotes the creation of a stable and retentive denture. Notably, the approach is patient-centric, placing equal importance on the precision of impression-making and ensuring long-term comfort during prosthesis use.
While the Modified Window Technique offers numerous advantages, it also presents certain challenges that clinicians must navigate:
-
Application challenges: One of the primary difficulties encountered with this technique is ensuring a consistent and controlled application of low-viscosity impression material on flabby tissues. This is particularly challenging due to gravitational forces, especially when working on the maxillary arch. Achieving uniformity becomes even more complex when considering the varied dental chair positions that might be adopted during the procedure.
-
Material selection and preferences: Many clinicians express a preference for PVS materials due to their versatility. PVS materials come in a range of viscosities, making them adaptable for both mucostatic and muco-compressive impressions of flabby ridges. This variability in viscosity allows clinicians to tailor their approach based on individual patient needs and specific clinical scenarios.
-
Sequential material usage: The technique often involves a two-step process with the use of both medium body and light body PVS. The medium-body PVS is utilized to create a compressive impression in areas outside of the flabby ridge. Subsequently, the light-body PVS is applied to capture finer details and ensure a stable, accurate impression.
In essence, while the Modified Window Technique offers innovative solutions to some of the challenges posed by flabby ridges, it also introduces complexities related to material selection and application. Clinicians must be adept at managing these intricacies to ensure optimal outcomes for their patients.
CONCLUSION
The innovative case report sheds light on the evolving landscape of prosthodontics, particularly concerning the management of flabby ridges. Traditionally, surgical removal of flabby tissue was seen as a primary solution. However, this approach has its drawbacks, prompting a search for alternative methods.
Several key points emerge from the case report:
-
Rethinking surgical solutions: There is a growing emphasis on moving away from surgical interventions like the removal of fibrous tissue. The drawbacks and potential risks associated with such surgeries have prompted clinicians to explore non-invasive alternatives.
-
Challenges with conventional techniques: The case report underscores the limitations of conventional impression methods, especially when dealing with unsupported tissue in the fabrication of removable complete dentures. These conventional techniques often fall short of capturing accurate impressions in challenging cases.
-
Treatment decision factors: The optimal treatment pathway is not one-size-fits-all. It is influenced by various factors such as the patient’s preferences, the current oral health condition, and their willingness to commit in terms of both time and finances.
-
Introducing the modified window technique: A pivotal aspect of the report is the introduction of the modified window technique. This innovative approach employs light-body PVS impression material in a controlled manner, aiming to tackle the challenges posed by flabby ridges. The technique offers the promise of improved accuracy without necessitating additional clinical visits.
-
Accessibility and cost-effectiveness: A noteworthy implication of the report is the potential democratization of treatment for flabby ridges. By suggesting that effective management can be achieved even in primary healthcare settings without resorting to surgical or implant-based solutions, the report hints at a more accessible and cost-effective approach to care.
In summary, the case report serves as a testament to the continuous evolution within prosthodontics. By highlighting innovative techniques and emphasizing patient-centric, non-invasive approaches, it paves the way for improved outcomes and broader accessibility in dental care.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors confirm that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of Artificial Intelligence (AI)-Assisted Technology for manuscript preparation
The authors confirm that there was no use of Artificial Intelligence (AI)-Assisted Technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Etiology and management of hypermobile mucosa overlying the residual alveolar ridge. J Prosthet Dent. 1974;32:619-38.
- [CrossRef] [PubMed] [Google Scholar]
- Management of the flabby ridge using a modified window technique and polyvinylsiloxane impression material. Saudi Dent J. 2018;30:89-93.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Prosthetic management of flabby ridge using customized prefabricated metal mesh custom tray impression technique: A case report. IP Ann Prosthodont Restor Dent. 2022;8:50-60.
- [Google Scholar]
- A review of prosthodontic management of fibrous ridges. Br Dent J. 2005;199:715-9.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical morbidity and sequelae of treatment with complete dentures. J Prosthet Dent. 1998;79:17-23.
- [CrossRef] [PubMed] [Google Scholar]
- Prosthodontic rehabilitation of patient with flabby ridges with different impression techniques. Indian J Dent. 2014;5:110-13.
- [CrossRef] [PubMed] [Google Scholar]
- Changes caused by a mandibular removable partial denture opposing a maxillary complete denture. J Prosthet Dent. 1972;27:140-50.
- [CrossRef] [PubMed] [Google Scholar]
- A single step impression technique of flabby ridges using monophase polyvinylsiloxane material: A case report. Case Rep Dent. 2014;2014:104541.
- [CrossRef] [PubMed] [Google Scholar]
- Impression of unsupported movable tissues. J Am Dent Assoc. 1981;103:590-2.
- [CrossRef] [PubMed] [Google Scholar]
- Modified impression technique for hyperplastic alveolar ridge. J Prosthet Dent. 1971;25:609-12.
- [CrossRef] [PubMed] [Google Scholar]
- Quality of written prescriptions and master impression for fixed and removable prosthodontics: A comparative study. Br Dent J. 2005;198:17-20.
- [CrossRef] [PubMed] [Google Scholar]
- Complete dentures from planning to problem solving. London: Quintessence Publishing; 2003. p. :123-133.
- Complete denturesda dental practitioner hand book. Bristol: Wright; 1986. p. :44-5.
- Removable denture prosthodontics (2nd ed). Edinburgh: Churchill Livingstone; 1992. p. :61.
- Management of the flabby ridge: A beleaguer for the prosthodontist! Dentistry Dent Pract J. 2022;5:1-3.
- [Google Scholar]
- Basic principles in impression making. J Prosthet Dent. 2005;93:503-8.
- [CrossRef] [PubMed] [Google Scholar]
- Management of the flabby ridge: Using contemporary materials to solve an old problem. Br Dent J. 2006;200:258-61.
- [CrossRef] [PubMed] [Google Scholar]
- The complete denture: A clinical pathway. Chicago: Quintessence; 1996. p. :7-15.
- A critical analysis of mid-century impression techniques for full dentures. J Prosthet Dent. 1951;1:472-91.
- [CrossRef] [PubMed] [Google Scholar]
- Complete denture secondary impression techniques to minimize distortion of ridge and border tissues. J Prosthet Dent. 1985;54:660-4.
- [CrossRef] [PubMed] [Google Scholar]
- The effect of seating velocity on pressure within impressions. J Prosthet Dent. 2008;100:384-9.
- [CrossRef] [PubMed] [Google Scholar]
- An analysis of the development of complete denture impression techniques. J Prosthet Dent. 1981;46:242-9.
- [CrossRef] [PubMed] [Google Scholar]
- Metaplastic formation of bone and chondroid in flabby ridges. Br J Oral Maxillofac Surg. 1986;24:300-5.
- [CrossRef] [PubMed] [Google Scholar]
- Oral status and prosthetic factors related to residual ridge resorption in elderly subjects. Acta Odontol Scand. 1997;55:306-13.
- [CrossRef] [PubMed] [Google Scholar]
- Designing complete dentures. P, Bristol: IOP Publishing; 1986. p. :21-34.
- Case report: Management of the flabby ridge: Re-visiting the principles of complete denture construction. In: Eur J Prosthodont Restor Dent. Vol 11. 2003. p. :145-8.
- [Google Scholar]
- Impression technique for maxillary fibrous ridge. Br Dent J. 1970;128:552.
- [CrossRef] [PubMed] [Google Scholar]
- A New presentation of combination syndrome. Annal Dent Univ Malaya. 2008;188:484-92.
- [Google Scholar]
- Management of flabby ridge in complete denture construction. Dent Update. 2005;32:524-8.
- [CrossRef] [PubMed] [Google Scholar]
- The management of flabby ridge in impression making for a complete denture. Stomatologis. 2010;67:171-6.
- [Google Scholar]
- Custom double tray for a special impression technique for flabby maxillary residual ridge: Case report. Clin Case Rep. 2022;10:e05593.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]







