Translate this page into:
POTENTIAL BIOLOGICAL AGENTS INVOLVED IN BIOTERRORISM - OBSERVATIONS FROM A DENTAL PERSPECTIVE
Corresponding Author : Dr. Deepak Viswanath
This article was originally published by Indira Gandhi Institute of Medical Science and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Bioterrorism can be described as the intentional use of microbiological agents or their toxins as weapons in a wide sense. The intentional release or dissemination of a biological warfare agent (BWA), such as bacteria, viruses, rickettsiae, fungi, or biological toxins, is considered bioterrorism. Terrorists and military services are drawn to BWAs because of their unique qualities, which make them ideal for use as warfare agents. Several elements influence the success of a bioterrorism attack. Two major criteria are the type of BWA and the target population.
Keywords
Bioterrorism
Biocrime
Epidemic
Pathogens
Biological Agents
INTRODUCTION:
Recent instances have made public health officials painfully aware of the significance of detecting bioterrorism quickly and properly. Because bioterrorism is difficult to foresee or prevent, it is critical to have dependable platforms in place to quickly detect and identify bioterrorism agents in order to limit the proliferation and widespread use of these agents and protect public health.1 These platforms must be sensitive, specific, and capable of detecting a wide range of pathogens directly from complicated sample matrices, including modified or previously uncharacterized agents. Recent laboratory prototype device inventions have been reviewed and commercialised. Various commercial assays that use biochemical, immunological, nucleic acid, and bioluminescence processes to identify biological threat substances are currently available. DNA aptamers, biochips, evanescent wave biosensors, cantilevers, living cells, and other new technologies have recently been created to identify bioterrorism agents.1
Bioterrorism and Bio-crime:
Bioterrorism, according to the CDC, is defined as the intentional release of viruses, bacteria, or other agents with the intent of causing illness or death in humans, animals, or plants. Bioterrorism is motivated by ideological, religious, or political ideas and seeks to cause casualties, terror, societal disruption, or economic damage. Terrorists, also known as nonstate actors, are responsible for it. Terrorists usually strive to achieve their objectives by instilling fear and violence. This terror could potentially be caused by bioterrorism.2
Last but not least, there's biocrime. This refers to the use of a biological toxin to kill or make sick a single person or a small group of people for the purpose of extortion or revenge, rather than political, ideological, religious, or other views. For example, a frustrated hospital laboratory employee used ricin to get rid of a partner in 1996, or a disgruntled hospital laboratory employee used Shigella dysenteriae to make pastries as a gift for her colleagues in 1996. The assassination of Hungarian dissident Georgi Markov in London in 1978 with a ricin laced pellet inserted through an umbrella could be classified as a biocrime. However, because the murder was very certainly intended to send a message to other dissidents on behalf of the KGB, one may argue that this is an example of state- driven BW.2
Types of Agents:
These agents are usually found in nature, but they could be changed or altered to boost their capacity to cause disease, make them resistant to current medications, or spread more easily.
| Category | Definition of Category | Disease | Organism(s)/Agent(s) |
|---|---|---|---|
| A | Organisms that pose a threat to national security are classified as high-priority agents because they: • Can easily be distributed or transmitted from person to person • Causes significant mortality and has the potential to have a major public health impact • Can generate public panic and communal disruption • Make public health preparedness a priority. |
Anthrax Botulism Plague Smallpox Tularemia Viral Hemorrhagic Fevers |
Bacillus Anthracis Clostridium botulinum toxin Yersinia pestis Variola major Francisella tularenis Filoviruses Arenaviruses |
| B | Agents with the second highest priority are those who: • Require specific laboratory diagnostic capability increases and better disease surveillance • Result in moderate morbidity rates and low mortality |
Brucellosis Epsilon toxin Food safety threats Glanders Melioidosis Psittacosis Q fever Ricin toxin Staphylococcal Enterotoxin B Typhus fever Viral encephalitis Water safety threats |
Brucella species Clostridium perfringens Salmonella species, Escherichia coli O157:H7, Shigella, and so forth Ricinus communis (castor beans) Ricinus communis Staphylococcus aureus Rickettsia prowazekii Alphaviruses (eg, Venezuelan equine encephalitis, eastern equine encephalitis, western equine encephalitis) Vibrio cholerae, Cryptosporidium parvum and so forth |
| C | Emerging pathogens, which could be developed for mass dispersion in the future, are the third highest priority agents, because of: • Availability • Ease of manufacture and transmission • High risk of morbidity and mortality, as well as serious health consequences |
Infectious diseases that are on the upsurge | Nipah virus Hantavirus Tick-borne hemorrhagic fever viruses Tick-borne encephalitis viruses Yellow fever Multidrug-resistant tuberculosis |
Adapted from Centers for Disease Control and Prevention. Bioterrorism Agents/Diseases.
Available at: http://www.bt.cdc.gov/agent/agentlist-category.asp. Accessed January 14, 2013.
Ref: Christian MD. Biowarfare and bioterrorism. Crit Care Clin. 2013 Jul;29(3):717-56. doi: 10.1016/j.ccc.2013.03.015. PMID: 23830660; PMCID: PMC7127345.
The agents listed in Table 1 were chosen because they have been weaponized for warfare or have been utilised in bioterrorism. These agents are the most likely to have a major impact and are hence the best suited.2
| Disease | Agent | Organism persistenc | Infective dose | Human to human transmiss ion | Infectivity | Incubati on period | Symptom | Mortality | Treatment |
|---|---|---|---|---|---|---|---|---|---|
| Anthrax | Spores of Bacillus Anthracis | Spores are extremely stable and can survive in soil for up to 40 years. | 8000- 50,000 spores | No | - | 1-6 days | Fatigue, fever, malaise, cough, mild chest discomfort, respiratory distress, shock | High | Ciprofloxa cin or doxycyclin e |
| Brucellosis | Genus Brucella | It will take 6 weeks. To 10 weeks in the dust. In the soil or in the water | 10-100 organisms | No | - | 5-60 days | Fever, headache, malaise, chills, sweating, myalgia, arthralgia, depression | 5% if left untreated | Doxycyclin e + Rifampicin |
| Glanders | Burkholder ia mallei | Highly stable | Unknown | Although uncommon, it is conceivable | - | 10-14 days | Pulmonary form: cough, chest pain, | ||
| Melioidosis | Burkholderia pseudomall ei | Highly stable | Unknown | Although ncommon, it is conceivable. | - | 10-14 days | fever, rigors, sweating, pleuritis | ||
| Plague | Yersinia pestis | In soil, it can last up to a year, although it is only viable for 1 hour after aerosol release. | 100- 20,000 organisms | High | Patients can be contagious for up to three days after beginning treatment. | 1-6 days | High fever, headache, malaise, chest pain, cough, haemoptysis, dyspnoea, stridor, cyanosis | ||
| Q-fever | Coxiella burnetii | heat and drying resistant, and it lasts for weeks to months. | 1-10 organisms | Although uncommon, it is conceivable. | 7-41 days | Fever, chills, headache, malaise, fatigue, anorexia, weight loss, endocarditis (as presenting symptom of chronic disease) | |||
| Salmonello sis | Genus Salmonella | resistant to heat up to 57-60°C | Unidentified | Faecal-oral transmission | In faeces for up to 4-5 weeks | 6-48 days | Nausea, vomiting, mucopurule nt or bloody diarrhoea, abdominal cramps, headache, maculopap ular exanthema | <1% | |
| Shigellosis | Genus Shigella | 2-3 days on average, up to 17 days in favorable conditions, several | 10-100 organisms | Feaecaloral transmission | There is a lot of excretion in the faeces during the acute phase; | 1-7 days | Fever, abdominal cramps, diarrhoea, haemorrhag ic colitis | <1% | |
| Tularemia | Francisella | hours on contaminat ed hands Years in |
10-50 | No | without antibiotic medicatio, it can extend up to 4 weeks. - |
1-25 | Fever, chills, | ||
| Smallpox | tularensis ssp. tularensis Variola virus: Variola major |
frozen meat, weeks in water, soil, or carcasses In dust and cloth, it can last up to a year. | organisms 10-100 organisms |
Yes, Close contact is required for transmission. | It is mostly infectious within the first | days 4-19 days 2-6 days |
myalgia, arthralgia, headache, nausea, vomiting, diarrhoea, sore throat Severe headache, high fever, extreme prostration, backache, |
<1% | |
| No | week after the rash emerges. | chest and join pains, anxiety, exanthema, maculopap | |||||||
| Venezualen Equine Encephalitis | Alphavirus, (Venezuelan equine | Unstable in its surroundings | 10-100 organisms | - | ular rash that becomes vesicular Malaise, spiking fevers, rigors, headache, myalgia, nausea, |
Ref: Jansen HJ, Breeveld FJ, Stijnis C, Grobusch MP. Biological warfare, bioterrorism, and biocrime. Clin
Microbiol Infect. 2014 Jun;20(6):488-96. doi: 10.1111/1469-0691.12699. PMID: 24890710; PMCID: PMC7129974.
IDENTIFICATION OF SPECIFIC DISEASES ASSOCIATED WITH BIOTERRORISM
This section gives an overview of the clinical and investigative data that can help in diagnosis of diseases. Laboratory testing, particularly microbiological studies, are essential for any biological diagnosis. The required specimens and assays for diagnosing possible bioterrorism agents are listed in Table 2. However, like with many elements of critical care, it's crucial not to rely on technology too much.
| AGENTS | CLINICAL SPECIMEN | AGNOSTIC TESTS | CHARACTERSTIC LAB FEATURES | BIOSAFETY LEVEL |
|---|---|---|---|---|
| Bacillus anthracis | Nasal swab Feces Lesion exudate A and C sera | Culture (nonhemolytic on 5% sheep blood agar, 35C, 18-24 h) FA Gammaphage anti-PA ELISA PCR and RT-PCR Capsule demonstration Immunochromatography | Gram-positive bacilli Spore-forming Nonhemolytic | 2 |
| Yersinia pestis | Nasal swab Sputum Bubo aspirate Blood A and C sera | Culture (5% sheep blood agar, chocolate agar, Casman blood agar, cystine heart blood agar, or MacConkey agar. 35C, 24-48 h) FA PCR RAD | Gram-negative coccobacilli Bipolar staining Nonlactose fermenter | 2 |
| Brucella sp | Whole blood Bone marrow A and C sera | Culture (tryptose agar with 5% bovine sera, Thayer-Marti n, chocolate agar with VCNT, 35C, 5%-10% CO2, 10 d) FA PCR | Gram-negative coccobacilli Aerobic Nonmotile Nonfermenter | 2 |
| Burkholderia sp | Whole blood A and C sera Lesion exudate | Culture (5% sheep blood agar, MacConkey agar. 35C, 24-48 h) PCR | Gram-negative bacilli Motile (except Burkholderia mallei) | 2 |
| Francisella tularensis | Nasal swab A and C sera | Culture (glucose cystine heart blood agar, thioglycolate, 35C, 48- 72 h) FA PCR | Gram-negative Obligate aerobe | 2 |
| Botulinum toxin | Nasal swab A and C sera | Immunoassay | 150 kDa protein neurotoxin | 2 |
| Ricin | Nasal swab A and C sera | Mouse neutralization | 66 kDa protein toxin | 2 |
| SEB | Nasal swab urine A and C sera | Antigen serology immunoassays | 23-29 kDa protein superantigens | 2 |
| Variola virus | Nasal swab Throat swab Lesion exudate A and C sera | Antigen serology immunoassays Viral culture* Electron microscopy PCR | Brick morphology | 4 |
| VEE Virus | Nasal swab Throat swab A and C sera | Viral culture Virus neutilization RT-PCR | Enveloped RNA Virus | 2 |
| VHF Virus | Nasal swab A and C sera | Viral culture* RT-PCR | Enveloped RNA Virus | 4 |
Abbreviations: A and C sera, acute and convalescent sera; ELISA, enzyme-linked immunosorbent assay; FA, fluorescent antibody; PA, protective antigen; PCR, polymerase chain reaction; RAD, rapid antigen detection kit; RT-PCR, real-time PCR; VCNT, vancomycin, colistin sulfate, nystatin, and trimethoprim; VEE, Venezuelan equine encephalitis.
*Not recommended except by qualified laboratory with appropriate biosafety equipment.
Adapted from Pavlin JA, Gilchrist MJ, Osweiler GD, et al. Diagnostic analyses of biologic agent-caused syndromes: laboratory and technical assistance. Emerg Med Clin North Am 2002;20(2):331-50; with permission.
DIAGNOSIS:
The most difficult phase in the response is likely to be diagnosing or identifying a bioterrorism event. There are two components to identifying a bioterrorism event:
Identifying that multiple episodes of disease were caused by a purposeful rather than natural phenomenon, and
Diagnosing the precise organism or substance that caused the illness. Depending on the conditions, they could happen in any order.
Recognizing a cluster of patients usually necessitates a level of situational awareness that is beyond the capabilities of a single doctor, and is usually only accessible by a regional, state, or federal public health agency, depending on how far dispersed the cases are.3
IDENTIFICATION OF A BIOTERRORISM EVENT VERSUS AN EPIDEMIC
Features that suggest a bioterrorism event rather than an epidemic
A curve that indicates a point source (common source) outbreak or an extended source rather than a naturally propagated (transmitted) source.
Determination of a group of cases (large numbers of patients from a similar geographic area with similar symptoms)
Case fatality is high and occurs quickly.
A substantial number of casualties within the first 48 to 72 hours following the strike (suggesting a microorganism attack) or within minutes to hours (suggesting a biological attack) (suggesting an attack with a toxin)
People who were indoors had a lower attack rate than those who were outside.
An extremely high proportion of respiratory involvement in disorders that usually result in a nonpulmonary condition when acquired naturally.
The distribution of casualties is coordinated with the direction of the wind.
A disease that is extremely uncommon in the area.
The onset of an illness classified as A, B, or C.
A rise in the number of sick or dead animals of various species in a specific geographic area.
Witness to an attack or the development of a suitable delivery method a Less trustworthy, because if a building's ventilation system was employed to spread the agent, the reverse may be true.
Data from Karwa M, Bronzert P, Kvetan V. Bioterrorism and critical care. Crit Care Clin 2003;19(2):280; and NATO Handbook on the Medical Aspects of NBC Defensive Operations, Part II-Biologic. Washington, DC: US Department of Defense, Department of the Army; 1996.
CHARACTERISTICS OF THE EPIDEMIC OF FEAR AND PANIC
Even when the agents cause low levels of death and physical morbidity, biological weapons attacks can have major emotional and societal consequences in a variety of ways. One of the initial mental impacts is a great deal of social and psychological suffering, particularly fear of biological agents, even when they aren't employed. This reaction can be attributed to a number of factors, including biological agents' invisibility, the likelihood that the agent can be disseminated through personal contact, the uncertainty around the magnitude of biological weapons' dangers, and so on. Exposure to any extreme stressor, whether natural event manmade, is, on the other hand, a risk factor for a variety of longterm social and mental issues.4
The epidemics of infectious disease and fear and panic are clearly depicted in Fig 1 with their numerical (number of cases) and chronological dimensions, as well as their zones of activity at each prevention level, emphasising the importance of primordial and primary prevention.4 It allows us to distinguish between the two types of epidemics in order to plan intervention strategies. At the individual and group level, the anticipation phase confronts fear, anxiety, and a probable lower level of panic and somatization. Activities aiming to minimise the anticipation phase of the fear and panic epidemic should be included at the primary and primary prevention levels.4
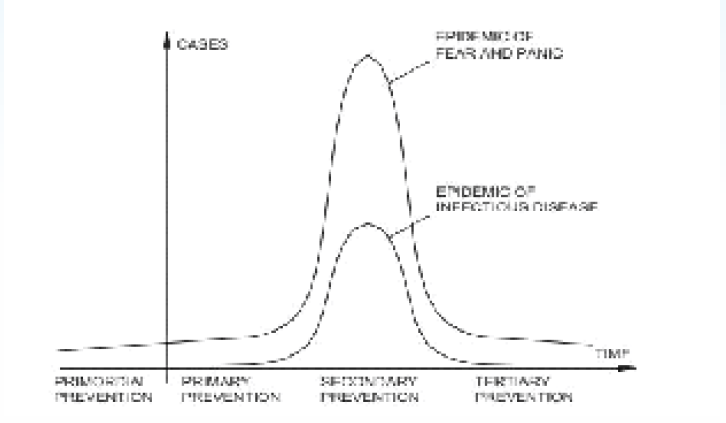
- Phases and levels of prevention of the epidemic of infectious disease and the epidemic of fear and panic.
- Ref: V. Radosavljevic et al Bioterrorism-Types of epidemics, new epidemiological paradigm and levels of prevention; Journal of royal institute of Public Health 121, 549-557; Elsevier; 2007
The second phase of the fear and panic epidemic happens at the same time as the infectious disease epidemic. People are interested in initiatives like as rescuing and helping because they are facing a real threat of infection. In this period, secondary prevention actions are recommended.4
Long after the attack, the level of anxiety and panic, as well as unpleasant mental health signs and symptoms, somatization, and grief, is greatly enhanced in the third phase. For the entire community, this is a time of great vulnerability. This is the time to take comprehensive tertiary preventative measures.4 Finally, we would like to contrast an infectious disease epidemic with a fear and panic epidemic induced by a bioterrorism attack (Fig. 1). Fear and panic epidemics begin at a higher level than infectious illness epidemics, have a significantly higher amplitude, and endure much longer due to the anticipation phase. While an infectious disease epidemic can last weeks or months, a fear and terror epidemic can endure months, if not years, and take on the characteristics of a pandemic.4
SURGICAL INDICATIONS AND THERAPY
There are no particular indications for surgical management of any bioterrorism pathogens, with the exception of perhaps cutaneous anthrax. Surgical debridement has been utilised primarily for injectable anthrax, even in the event of anthrax.3
SUPPORTIVE CARE AND RESPONSE
Basic care of the individual patient and the response to a mass casualty event are two aspects of supportive care for victims of bioterrorism. Despite increased awareness of the threat of bioterrorism after 2001, many hospitals are still unprepared for biological attacks. According to a study of UK emergency departments (EDs), 24% lacked isolation facilities, and just 61 percent had departments with independent ventilation systems, permitting the unit to be isolated from the rest of the hospital.3
The Task Force for Emergency Mass Critical Care offers hospitals with instructions for preparing for and managing mass critically sick casualties in the event of a bioterrorism strike. These guidelines should be familiar to critical care physicians, and they should be prepared to respond in such situations, because if they are not, all of their talents and knowledge for treating individual patients will be useless when the system gets overwhelmed.3
Individual patient support can be divided into three groups according on the type of agent involved: bacterial, viral, or toxin. Bacterial and viral pathogens commonly cause sepsis with vascular leak, especially in the event of VHF, as well as varying degrees of systemic inflammatory response.3
Supportive therapy for patients exposed to bio-toxins in bioterrorism incidents differs depending on the toxin. The primary support necessary in the case of botulinum toxin exposure is mechanical breathing, hydration, and nutritional support until the paralysis resolves. Both ricin and mycotoxins function at the cellular level, and while supportive therapy should be tried, they may be ineffective in changing patient outcomes. In the case of mycotoxins, the administration of steroids as part of supportive care may be beneficial.3
EXACT ROLE FOR DENTISTRY?
Dental surgeons can play a critical part in the planning of a bioterrorism strike and its subsequent response, resulting in a positive outcome. Local demands could be immediate and massive in the event of a significant bioterrorism strike. As hospitals grow overburdened, alternative locations for providing health care will be needed, and dentist offices and hospitals may be able to serve that demand.6

Table 3: Thus a dentist/dental surgeon can work towards7
Ref: Yogeshwari, Agarwal A, Aeran H. The role of a dental surgeon during a bioterrorism attack. Int J Oral Health Dent 2020;6(2):66-70
Therefore, the prime role of the dentists are as follows:
Assistance during an attack: Depending on the community's needs and available resources, dentists and other dental workers may be able to assist during the initial few days of a potential bioterrorist strike. These can range from individually packaging pharmaceuticals to providing a major percentage of primary medical treatment in a sequestered region if doctors are unavailable due to disability or death.7
Surveillance and Notification: Disease surveillance systems are essential not just for detecting an outbreak early on, but also for monitoring the outbreak's scope and progress and determining when it is over. Gathering information from contact tracing and exposure source investigations, as well as information on important medicine, medical equipment availability, and managing corpses, would be necessary for managing a significant outbreak.7
It may be difficult to identify the real perpetrator of a bioterrorist strike since diseases employed as weapons in bioterrorist operations have an incubation time before clinical signs appear. Dentists are a great monitoring resource because they may recognise and report typical intraoral or cutaneous lesions to public health authorities when they occur. These may also be able to discover unusual patterns of staff or patient cancellations or missed appointments that aren't explained by known local factors.7
Referral: Dentists might refer worrisome conditions to experts for confirmation, treatment, or both. Immunizations, triage facilities, improved medical care, decontamination, and infection control are all important areas to focus on.7
DENTIST OR A DENTAL SPECIALIST ROLE IN DIAGNOSING OR CURBING BIO TERRORISM
Recognizing the urgency to establish dentistry's participation in a bioterrorist attack, the American Dental Association (ADA) held a workshop in June 2001 that was attended by renowned bioterrorism experts. It was one of the first attempts to get a consensus on the function of dentistry in these situations. The American Dental Association and the US Public Health Service co-sponsored a seminar in March 2003 on "Dentistry's Role in Responding to Bioterrorism and Other Catastrophic Events."8
Organized dentistry and dental educators must work together to establish training programmes that take advantage of dentists' medical and scientific knowledge as well as clinical patient care skills. Programs to teach general dentists in emergency preparedness and to train trainers to train other health-care professionals in emergency response and public health awareness are already in the works.8
Dentists can actually shield themselves, their patients, and the community by providing a trustworthy and scientifically correct source of information before, during, and after a biological emergency. Dentists can operate as sentinels for early detection of illness outbreaks, whether they arise spontaneously or as a result of the actions of individuals with malicious intent, given to their understanding of fundamental medicine and particular competence in oropharyngeal diseases.8
Local dental societies and individuals must issue an invitation to incorporate community dental assets into local emergency response plans, bringing not just the dentist's talents but also the skills of well-trained ancillary people. Most cities' dispersed dental office distribution patterns make them ideal candidates for community-based distribution or immunisation centres, potentially alleviating some of the pressure on hospitals and medical centres.8
Dentists may be required to give care outside of the typical boundaries specified by state dental health care acts if they are fully integrated into disaster response operations. Training, certification, scope of service, and liability protection for appropriately trained responding dentists must be discussed by dental academia, organizational dentistry, state legislators, and federal and state politicians.8
If the necessity arises, dental offices equipped with highly valued equipment will be able to serve as regional auxiliary hospitals. Educational programmes on potential biological weapons, as well as continuing education courses, should be designed as part of the dentistry school knowledge.7
Incorporating Bioterrorism Training into the Dental Curriculum
The following are three basic strategies for incorporating terrorist training into the pre-doctoral dentistry school curriculum: 9
In the first scenario, a new course or courses/study material should be added to the dental curricula to overcome the gap of knowledge and willingness.
Bioterrorism training can also be smoothly included into existing likewise only as a new chapter can be added to the already existing courses. Also, Different parts of identifying and diagnosing related newer methods of training can be introduced into the curriculum in this scenario without interrupting the curriculum's framework.
The third scenario, we can merge the above two methods.
CHALLENGES AND CONSIDERATIONS
Regional heterogeneity, administration of the fundamental scientific curriculum, and cost considerations are all obstacles to introducing bioterrorism training into the dentistry school curriculum.9
First, while a terrorism attack can certainly occur throughout the country, certain regions are more likely to face such an event than others. Dental schools in regions less likely to be the target of an attack may be less interested in devoting curriculum time to training dental students to respond to an attack. Incorporating training into the current curriculum, rather than creating new courses, may provide the best option for dental schools located in more likely target areas, yet barriers may remain at dental schools in rural and other areas considered unlikely to be prime targets of terrorism.9
Second, in institutions where the basic sciences are taught in a separate school or in conjunction with the medical school, incorporating emergency response and bioterrorism training into the existing curriculum may necessitate an extra effort of coordination and cooperation.9
Finally, implementing changes into the curriculum can necessitate a large investment of time and money. Allocating the necessary resources to the establishment of a terrorism training curriculum may prove problematic in a time when dental schools are suffering major funding constraints. All potential funding sources, including grants, must be thoroughly investigated. It should also be explored developing an exportable package that could be supplied to dental institutions and used to instruct dental students.9
CONCLUSIONS:
Bioterrorism, or BW, isn't a new threat, and it's not going away anytime soon. Given the technological obstacles and limits imposed by the necessity to work in secret, the possibility of a successful bioterrorist assault is minimal, and more likely at the low- technology end of the spectrum than at the hightechnology end. Even if the number of casualties is likely to be low, the impact of a bioterrorist assault can be significant, affecting many lives and causing significant direct and indirect costs. As a result, it is better to be prepared to deal with the ramifications. The role of dentistry in reacting to bioterrorism and other catastrophic occurrences is changing and could include a variety of activities. Local emergency response planners should be made aware of the services the dental profession can provide, and dental resources should be integrated to strengthen the disaster response capacity of community health care systems, according to organised dentistry, local dental societies, and interested individuals.
REFERENCES:
- Biosensors for Security and Bioterrorism: Definitions, History, Types of Agents, New Trends and Applications. 2016 10.1007/9783-319-28926-7_1
- [Google Scholar]
- Biological warfare, bioterrorism, and biocrime. Clin Microbiol Infect. 2014;20(6):488-96.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Biowarfare and bioterrorism. Crit Care Clin. 2013;29(3):717-56.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Bioterrorism-Types of epidemics, new epidemiological paradigm and levels of prevention; Journal of royal institute of Public Health. Vol 121. Elsevier; 2007. p. :549-557.
- [CrossRef] [PubMed] [Google Scholar]
- Mining Candidate Viruses as Potential Bio-terrorism Weapons. 2005:60-71. ISI 2005, LNCS 3495
- [CrossRef] [Google Scholar]
- The role of a dental surgeon during a bioterrorism attack. Int J Oral Health Dent. 2020;6(2):66-70.
- [CrossRef] [Google Scholar]
- Managing Bio-Disaster: Role of Dentist | Manohar Parrikar Institute for Defence Studies and Analyses. . 2019;12(4)
- [Google Scholar]
- Dentistry and bioterrorism. Dent Clin North Am. 2003;47(4):733-44.
- [CrossRef] [PubMed] [Google Scholar]
- Incorporating Bioterrorism Training into Dental Education: Report of ADA-ADEA Terrorism and Mass Casualty Curriculum Development Workshop. Journal of Dental Education. 2004;68(11)
- [CrossRef] [PubMed] [Google Scholar]







