Translate this page into:
Mitigating Musculoskeletal Occupational Hazards in Dentistry: Strategies for Prevention and Well-Being

*Corresponding author: Dr. Nitika Naryal, Department of Public Health Dentistry, Himachal Pradesh Government Dental College and Hospital, Shimla, India. nikiesunvij01@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Naryal N, Bhardwaj V, Fotedar S, Thakur AS, Vashisth S, Mitigating Musculoskeletal Occupational Hazards in Dentistry: Strategies for Prevention and Well-being. Dent J Indira Gandhi Int Med Sci. 2025;4:17-20. doi: 10.25259/DJIGIMS_24_2024
Abstract
A collection of illnesses or injuries affecting the nerves, muscles, tendons, bones, joints, cartilage, and intervertebral discs are referred to as musculoskeletal disorders (MSDs). Dentists are more likely to develop work-related MSDs, which can result in unsuitable positions during work for extended periods, repetitive, unnatural motions, genetic predisposition, aging, and mental pressure. Common MSDs include tension neck syndrome, cervical radiculopathy, back pain syndrome, and carpel tunnel syndrome. More than one-third of dentists seek medical assistance for these MSDs, which have an impact on their daily and professional lives. Therefore, the present review article aims to address and discuss the common musculoskeletal hazards faced by dental professionals and emphasizes the importance of a holistic approach and effective strategies for prevention and promoting the well-being of dental professionals.
Keywords
Dentistry
Ergonomics
Musculoskeletal disorders
Occupational hazard
Prevention
INTRODUCTION
Illnesses or injuries affecting the nerves, muscles, tendons, bones, joints, cartilage, and intervertebral discs collectively are referred to as musculoskeletal disorders (MSDs). They cause one of the biggest losses of years of productive life, which often leads to an early retirement due to functional, mental, and physical limitations.[1]
A prolonged amount of time spent in improper positions and repetitive aberrant motions overstress the peripheral nerve system, the spine, and limbs, which in turn increases the risk of developing musculoskeletal pain in the neck, shoulder, lower limbs, hands and wrists, and back.[2] It happens because of the small work area related to the oral cavity due to which a dentist often adopts uncomfortable body positions to obtain good access and visibility.[1] MSDs commonly affecting dentists include tension neck syndrome, cervical radiculopathy, back pain syndrome, and carpal tunnel syndrome (CTS), which influence dentists’ daily and professional lives.[2]
Therefore, the present review article aims to address and discuss the common musculoskeletal hazards faced by dental professionals and emphasizes the importance of a holistic approach and effective strategies for prevention and promoting well-being.
MUSCULOSKELETAL HAZARDS IN DENTISTRY
In order to reach the narrow intraoral area, dentists typically adopt bad posture, which strains their rotator cuff tendons, periscapular muscles, and upper extremity musculoskeletal systems. It is often necessary to hold this position between four and thirty seconds on a regular basis in clinical treatments to increase visibility for hand dexterity and the best possible eye-hand synergy.[3]
The dentist can only tilt the head more than 65° and the body between 20° and 25° when employing the direct view technique; these angles might be 38° and 5°, respectively, while employing the mirror view approach.[4] Figure 1 demonstrates that although neck flexion decreased when using the mirror view approach, it is still greater than the recommended ergonomic requirements (i.e., >20°), posing a serious risk to dentists’ cervical spines.[4]

- Poor working posture in dentistry.
The muscles in the neck and back must contract regularly to support the weight of the head against gravity because of the forward-head posture. Axial neck discomfort, sometimes referred to as “tension neck syndrome,” may result from this. This condition can cause chronic pain in the neck, posterior head, and periscapular muscles. Rarely, it may even radiate into the shoulders and arms.[3,4]
Cervical spondylosis is associated with an increased risk of cervical radiculopathy. Cervical radiculopathy can result from compression of the cervical nerve root caused by either bony osteophytes impinging on the nerve root or cervical intervertebral disc herniation, as depicted in Figure 2.[5] Since intervertebral discs lack blood arteries, diffusion from these veins is the only source of nutrition for them. An efficient pump mechanism nourishes the intervertebral discs and is stimulated by the disc’s periodic transition between high and low loads or movement (during posture alteration). However, this is not the case when one maintains a lengthy static position, as this reduces disc nourishment and causes degenerative changes.[6]
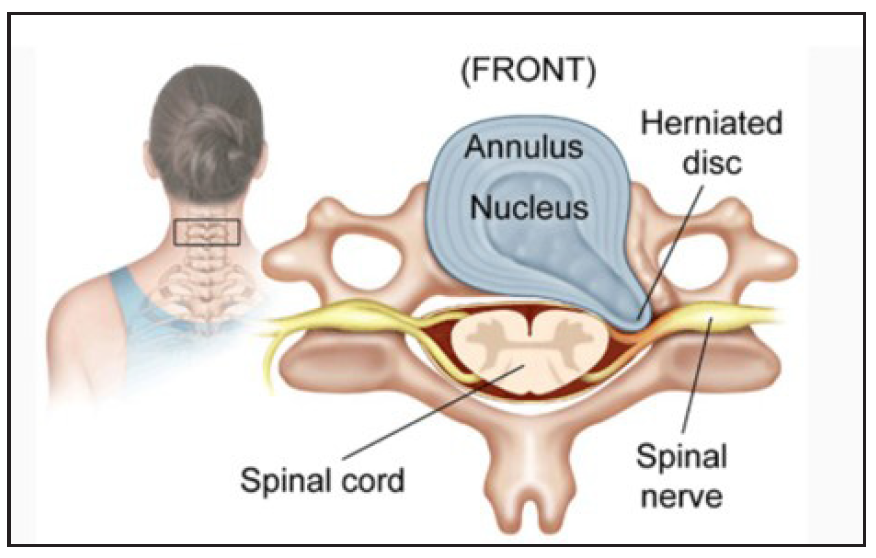
- Herniated disk in the cervical spine.
The most frequently damaged nerve roots are the C7 root (C6-7 herniation), which is followed by the C6 (C5-6 herniation) and C8 (C7-T1 herniation) nerve roots. Mechanical compression of the nerve probably causes localized ischemia and nerve injury, which manifest as pain, numbness, or tingling in specific locations.[7]
Age-related degenerative alterations in the cervical spine are referred to as cervical spondylosis. In such situations, foraminal constriction and decreased disc height are caused by degradation of the disc with age. Decreased disc height leads to increased loads to the vertebral body and the intervertebral joints. This consequently results in bony hypertrophy. Further, foraminal stenosis and cervical radiculopathy are caused by hypertrophy of the uncinate joint.[3]
The back muscles inhibit anterior bending; however, during prolonged or repetitive bending actions, muscular protection may be lost, most likely due to creep deformation in spinal receptors that effectively eliminates the protective muscle reflex. When excessive bending and compression are applied to the lumbar spine at the same time, the intervertebral disc posteriorly prolapses and causes chronic lower back pain.[3]
The carpal tunnel is the result of the flexor retinaculum and carpal bones forming a deep arch anteriorly at the wrist. The median nerve, along with the four tendons of the flexor digitorum profundus, flexor digitorum superficialis, and flexor pollicis longus, all pass through the carpal tunnel. An entrapment syndrome called CTS is brought on by pressure on the median nerve inside the carpal tunnel.[8]
Repetitive hand motion, awkward hand position, strong gripping, mechanical stress on the palm, and vibration are ergonomic risk factors associated with CTS. These risk factors, when presented to the dentist, result in contact stress over the carpal tunnel and wrist, leading to muscular atrophy, ultimately progressing to CTS, as shown in Figure 3.[8]
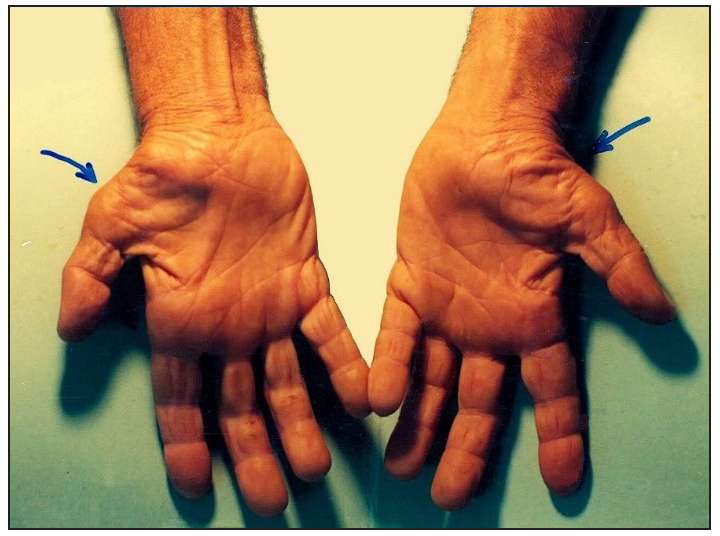
- Blue arrows in the image shows muscular atrophy of carpal tunnel and wrist area in carpal tunnel syndrome.
Loss of touch, tingling, and numbness in the hand and fingers, shoulder pain at night, elbow or wrist pain, loss of hand grip strength, and wrist pain when stretched in an extreme posture are some of the symptoms of CTS.[8]
STRATEGIES FOR PREVENTION
Engineering controls at the workplace are designed to reduce awkward positions as much as possible and utilize ergonomically designed furniture and equipment. The dentist’s and patient’s chairs should be adjusted to a comfortable height with lumbar, thoracic, or arm support. The instrument table should be positioned appropriately, and the workspace should have enough lighting, ventilation, and a suitable temperature.[9]
The patient should be in a supine position, and the chair should be lifted to allow the operator’s thighs to rotate freely below the patient’s chair in order to preserve a neutral posture. The patient’s head should have enough clearance for right-handed operators to move freely between the 7 and 12:30 positions.[9] For most intraoral access sites, the maxillary plane should be 7° beyond the vertical. To treat the maxillary second and third molars, the maxillary plane should be 25° above the vertical. The maxillary plane should be 8° forward of the vertical for the mandibular anterior teeth when the patient’s chin is down.[9]
Instead of using manual hand instruments, practitioners should think about using belt-driven drills, lasers, ultrasonic scalers, endodontic handpieces, and lightweight, balanced, high-speed handpieces.[10] Round handles with shallow, circumferential grooves provide improved friction with the fingertips, reducing the effort needed for a secure grip and reducing digital nerve compression and muscle strain. The instrument does more work when the working edges are sharp, but more operator force is needed to accomplish the same task when the edges are dull. Therefore, in order to avoid excessive force during instrumentation, sharp instruments are preferred.[10]
When practicing four-handed dentistry, the dentist should keep their eyes focused on the working field and maintain a position around the operating field with little movement of their own hands, arms, or torso. From an ergonomic perspective, dental assistants can more easily access the handpieces for bur changes and other instruments for procedures when using over-the-head and over-the-patient delivery systems.[9] Low finger temperature can be caused by a variety of factors in the workplace, including exposure to cold air exhaust, handling cold objects or materials, and low room temperatures. Although there are no set guidelines for finger temperatures, it is advised that hands and fingers are to be kept above 25° C or 77° F to prevent negative impacts on grip strength and dexterity.[9]
Even shadow-free, color-corrected illumination focused on the operational field is the aim of overhead lighting. Generally speaking, there should be no more than a 3 to 1.6 intensity ratio between ambient room lighting and task illumination (the dental operating light). In addition, the light source needs to be positioned in the mid-sagittal plane of the patient, 5° toward the operator’s head at the 12 o’clock position, directly above and slightly behind the patient’s oral cavity.[11]
Administrative controls are those that concentrate on the organization and work performance, including creating ergonomic standards for tools and equipment, testing new tools and equipment with worker input through user trials, maintaining tools and equipment to maximize performance, offering training programs to inform workers about risk factors and safe work practices, and promoting early detection and reporting of MSD symptoms.[9]
The most crucial piece of personal protective equipment for reducing ergonomic risks is suitable footwear with supportive and grippy soles. Every oral healthcare provider needs to wear gloves that fit and are the right size. While the impact of gloves on hand discomfort remains unexplored, they have been suggested as a possible indirect cause of CTS.[11]
DISCUSSION
MSDs show a high prevalence among dental professionals, which ranged from 10.8%–97.9%.[12] MSDs in dentistry commonly present as back pain, neck and shoulder discomfort, and pain in the hand and wrist region, which occur due to inadequate ergonomic practices, such as slouching or leaning forward, prolonged sitting or leaning forward or tilting head downward and forward, holding the same position for extended periods, reaching and holding arms in an elevated position, repetitive movements and forceful gripping of hand instruments and dental tools, and improper design of equipment such as nonergonomic dental chairs, stools, and instruments.[12] According to Leitz et al.’s systematic analysis,[12] the neck (58.5%) was the body part most frequently afflicted, followed by the lower back (56.4%), shoulder (43.1%), and upper back (41.1%).
Numerous studies have examined the impact of various ergonomic solutions on the prevalence and severity of MSDs as well as dental professionals’ working posture [10,13,14] and these studies have shown that the use of lightweight dental instruments with a wide diameter reduced shoulder discomfort symptoms, the use of loupes improved upper extremity pain and disability, and the use of an ergonomic dental chair with arm support improved dentists’ working posture. The well-being of dental professionals can be promoted by increasing awareness about the importance of musculoskeletal health through regular training sessions on ergonomics and proper posture techniques, encouraging regular physical activity and exercises to strengthen core muscles and improve overall fitness, addressing stress and mental health issues through mindful practices, and promoting a healthy work–life balance to reduce the overall physical and mental strain.[15]
CONCLUSION
Mitigating musculoskeletal occupational hazards in dentistry requires a comprehensive approach that includes ergonomic interventions, proper posture and movement practices, optimization of the work environment, ongoing education, and promoting overall well-being. By implementing these strategies, dental professionals can significantly reduce the risk of MSDs, enhancing their health, productivity, and quality of life. Further research is needed to develop innovative ergonomic solutions and interventions tailored specifically for dental professionals. In addition, longitudinal studies can help in understanding the long-term benefits of preventive strategies and their impact on reducing MSDs in dentistry.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent is not required as there are no patients in this study.
Financial support and sponsorship
Nil
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
REFERENCES
- Musculoskeletal disorders among dentists and variation in dental work. Appl Ergon. 1998;29:119-25.
- [CrossRef] [PubMed] [Google Scholar]
- Occupational hazards among clinical dental staff. J Contemp Dent Pract. 2004;5:134-52.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of line of vision on posture, muscle activity and sitting balance during tooth preparation. Int Dent J. 2021;71:399-406.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Caring for the neck and posture in dentistry: better late than never. Int Dent J. 2022;72:150-3.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Risk for cervical herniated intervertebral disc in dentists: A nationwide population-based study. BMC Musculoskelet Disord. 2019;20:189.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Genetics of disc-related disorders: Current findings and lessons from other complex diseases. Eur Spine J. 2014;23:S354-63.
- [CrossRef] [PubMed] [Google Scholar]
- Mechanical initiation of intervertebral disc degeneration. Spine (Phila Pa 1976). 2000;25:1625-36.
- [CrossRef] [PubMed] [Google Scholar]
- Ergonomic risk and preventive measures of musculoskeletal disorders in the dentistry environment: An umbrella review. PeerJ. 2018;6:e4154.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The effects of periodontal curette handle weight and diameter on arm pain: A four-month randomized controlled trial. J Am Dent Assoc. 2012;143:1105-13.
- [CrossRef] [PubMed] [Google Scholar]
- Prevention of work-related musculoskeletal disorders among dental professionals: A scoping review. Work. 2022;72:91-108.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence and occupational risk factors of musculoskeletal diseases and pain among dental professionals in Western countries: A systematic literature review and meta-analysis. PLoS One. 2018;13:e0208628.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The effect of wearing loupes on upper extremity musculoskeletal disorders among dental hygienists. Int J Dent Hyg. 2014;12:174-9.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of prismatic glasses including optometric correction on head and neck kinematics, perceived exertion and comfort during dental work in the oral cavity--a randomised controlled intervention. Appl Ergon. 2012;43:246-53.
- [CrossRef] [PubMed] [Google Scholar]
- Investigating the effect of educational intervention on musculoskeletal disorders in dentists. World Fam Med. 2018;16:307-13.
- [CrossRef] [Google Scholar]








