Translate this page into:
ACANTHOMATOUS AMELOBLASTOMA IN ANTERIOR MANDIBULAR REGION: A RARE CASE REPORT
Corresponding Author : Ajay Kumar
This article was originally published by Indira Gandhi Institute of Medical Science and was migrated to Scientific Scholar after the change of Publisher.
Abstract
After odontoma, ameloblastoma is the second most common odontogenic tumor. Ameloblastoma is locally aggressive and exhibit high tendency of recurrence. It arises from the remnants of odontogenic epithelium, odontogenic cystic lining and the basal layer of the oral mucosa. Ameloblastoma accounts for 1% of all odontogenic cyst and tumors, and 9-11% of various odontogenic tumors of the jaw. There is no sex predilection, it affects both the genders equally, and male to female ratio is 1:1. Clinically it present as painless, slow-growing odontogenic tumor, usually involves mandibular posterior region. There are several histological varieties of ameloblastoma but the acanthomatous variety being one of the rarest. We present a case of acanthomatous ameloblastoma involving mandibular anterior region.
Keywords
Ameloblastoma
Acanthomatous
Odontogenic
benign tumour.
INTRODUCTION:
The term "Ameloblastoma" is the combination of two word "amel" which mean enamel and "blastos" which means the germ.1 The tumor originates principally from the remnants of dental lamina.
Historically, the first description of ameloblastoma reported by Cusack in 1827. Later in 1885, the term "adamantinoma" was introduced to the literature. Ivey and Churchill in 1930 coined the term "Ameloblastoma". The most accepted definition of ameloblastoma was given by Robinson in 1937, as "usually unicentric, nonfunctional, intermittent in growth, anatomically benign and clinically persistent."1 The World Health Organization (WHO) (1991) defined ameloblastoma as a benign but locally aggressive tumor with a high tendency to recur, consisting of proliferating odontogenic epithelium lying in a fibrous stroma.2
It is considered to be odontogenic tumour of epithelial tissue, principally of enamel organ-type, lacking the differentiation to the point of hard tissue formation. Mutations in genes that belong to MAPK pathway (most common mutation is the BRAFV600E) have been discovered in genetic studies of many ameloblastomas.3
World health organisation in 2005 classifies ameloblastoma into for category of solid / multicystic, extraosseous / peripheral, desmoplastic and unicystic types. Currently in 2017, two modifications has been undertaken-a) The term "solid/multicystic" was removed because of its no biologic significance and the confusion with unicystic ameloblastoma b) Desmoplastic ameloblastoma removed from the clinical classification and reclassified as a histological subtype. Thus the new clinical subtypes of ameloblastoma are conventional ameloblastoma, Unicystic ameloblastoma and peripheral / extraosseous ameloblastoma.4
Here, we are reporting a case of acanthomatous ameloblastoma of anterior mandible, crossing the midline, which is rarest of its own.
CASE REPORT:
A 63-year-old male patient came to the department of oral and maxillofacial surgery at Dental College Azamgarh with a chief complaint of swelling in his lower front region of the jaw. (Figure 1) The swelling was gradual in onset, and slow growing. There was positive history of trauma 4 year back with negative history of any toothache, or any reduction in the size of the swelling, paresthesia and discharge. Only little discomfort was reported during biting food.

- Extra oral photograph of patient showing diffuse swelling over the anterior mandibular region
On clinical examination, a solitary diffuse swelling over the anterior mandibular region, measuring approximately 4×5 cm was present. (Figure 1). The skin overlying was stretched, smooth and normal in color with no other significant findings. It was firm and non-tender on palpation.
On intraoral examination, a solitary swelling in the lower vestibule region with vestibular obliteration in relation with 44, 43, 42, 41, 31, 32, 33 and 34, measuring approximately 3.5×4.5 cm was present. Mucosa overlying was smooth, stretched and normal in color. On palpation, it was soft to firm in consistency and non-tender. Based on clinical examination, a provisional diagnosis of radicular cyst was given. Central giant cell granuloma, periapical cemental dysplasia and ameloblastoma were given as differential diagnosis. On vitality testing, the tooth was vital. On FNAC, the straw color fluid was seen. (Figure 2)

- FNAC- Straw colour fluid Aspirated
On radiographic examination, panoramic radiograph revealed well defined unilocular radiolucency in the periapical region of 44, 43, 42, 41, 31, 32, 33, and 34 measuring about 4×2.5cm, extending mesio-distally from mesial of 45 to the distal of 35 and supero- inferiorly from alveolar crest to the 0.8mm superior to the lower border of mandible in the 42, 43 regions. The internal structure was completely radiolucent. Root resorption is present in relation with 44, 43 and 42.(Figure 3).

- Panoramic radiograph showing unilocular radiolucency in relation with 44, 43, 42, 41, 31, 32, 33 and 34.
CBCT scan revealed a well-defined hypodensity measuring 4.1×2.4cm in relation with the periapical region of 44, 43, 42, 41, 31, 32, 33 and 34. (Figure 4) The borders of the pathology are well-defined and non-corticated, internal structure of the pathology is totally hypodense. Perforation of the labial cortical plate is noted. (Figure 5) Root resorption is noted with respect to 31, 32, 33, 41, 42 and 43. Based on radiological feature, radiological diagnosis of infected periapical cyst in relation with mandibular anterior region was given, and radiological differential diagnosis of unicystic ameloblastoma was given.

- CBCT View showing well -defined hypo-density in relation with 44, 43, 42, 41, 31, 32, 33 and 34.
- Axial section and oblique coronal section of CBCT showing well-defined hypo-density with labial plate perforation.
The FNAC report showed presence of polymorphs, lymphocytes, histiocytes and degenerated cells in a hemorrhagic background with occasional squamous cells. No malignant cells were seen. Incisional Upon biopsy, there were solid epithelial nests with peripheral palisading ameloblastic cells and a central squamous metaplasia consistent with an acanthomatous ameloblastoma. (Figure 6).
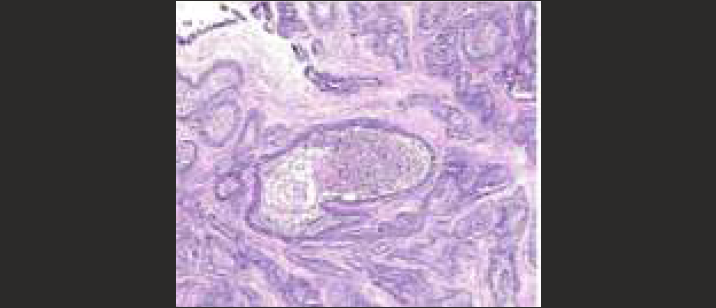
- Histopathological view showing solid epithelial nests with peripheral palisading ameloblastic cells and central squamous metaplasia
After obtaining the consent from the patient and routine blood investigations, the surgery was performed under local anesthesia. A crevicular incision was made to disclose the pathology and enucleation of the lesion as a conservative surgery was performed with removal of upto 5 mm of bone with round bur including surrounding healthy bone (Figure 7).
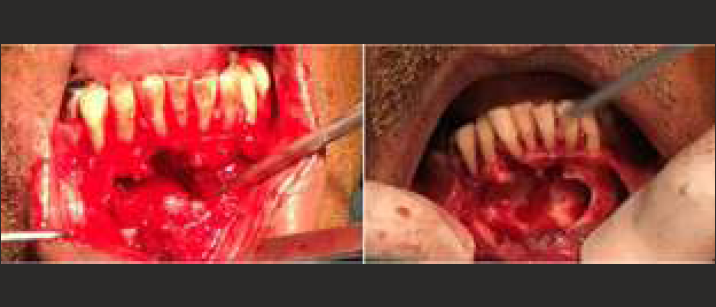
- Enucleation of the lesion with removal of 1 to 2mm of bone
The application of Carnoy's solution after conservative excision was done. Following the excised specimen's histological examination, acanthomatous ameloblastoma was confirmed (Figure 8). Post operative follow up did not show any adverse complications. (Figure 9). Patient was kept under periodic follow-up to check for any recurrence. A post operative radiograph made after 2 year showed healing lesion with bone formation.

- Excisional biopsy samples

- Post operative panoramic radiograph after 2 years showing post surgical healing
DISCUSSION:
Ameloblastoma is benign origin, arises from remnants of odontogenic epithelium, dental lamina or enamel organ and exhibits high recurrence rate. If it is left untreated, it exhibits destruction and deformity due to it local aggressive and invasive behavior.1,2
Usually ameloblastoma occurs during third to fifth decade, but in contradictory acanthomatous ameloblastoma found to be many in seventh decade of life.5 In our case the acanthomatous ameloblastoma reported in a patient of 6th decade of life.
It can occur both in maxilla or mandible but most commonly it occurs in mandible (about 80% of the cases) in posterior region. Out of 80% of ameloblastoma, 70% are located in the area of the ascending ramus or the molars.5 In contrast to this, our case reported with the lesion in the mandibular anterior region, which is rare and was also crossing the midline
Clinically, ameloblastoma is slow growing, painless swelling with expansion in buccolingual direction. The lesion can grow enormously, lead to facial deformity, malocclusion, loosening of teeth, perforation, soft tissue invasion and paresthesia.5,6 There was significant labial cortical plate destruction with root resorption in our case.
Chair side investigation usually includes fine needle aspiration cytology (FNAC). Usually FNAC can results in different fluid on aspiration such as straw colored, white thick creamy, blood or pus and sometime air. Ameloblastoma usually gives either straw colored fluid or negative results on aspiration based on different subtype. Our case we aspirated straw colored fluid which was suggestive of cystic changes.7 Different modalities of imaging investigations can be performed to evaluate and assess the pathology such as periapical, occlusal, panoramic, cone beam computed tomography (CBCT), computed tomography (CT), and magnetic resonance imaging (MRI). CT and CBCT usually help radiologist to evaluate the bone characteristics, while MRI is helpful in providing details of soft tissues which get involved by the lesion.8
Radiographically, ameloblastoma present as either unilocular or multilocular radiolucency. Conventional ameloblastoma usually presents with multilocular radiolucency due to the presence of bony septa creating internal compartments. Initially these internal compartments are smaller giving honeycomb appearance; later the compartments become bigger and lead to soap bubble appearance. On the other hand unicystic ameloblastoma present as unilocular radiolucency, which can be misdiagnosed as radicular cyst. It can also show expansion, displacement of the teeth with knife edge root resorption radiographically.7,9 In our case, panoramic and cone beam computed tomography (CBCT) revealed well defined unilocular, non-corticated radiolucency directing toward unicystic ameloblastoma radiographically.
Histopathologically, the follicular and plexiform patterns are the most common whereas acanthomatous ameloblastoma is one of the rare types.8 According to Adebiyi et al, the most common histopathological type reported is follicular (64.9%), followed by plexiform (13.0%), desmoplastic (5.2%) and least acanthomatous (3.9%).9 Acanthomatous type, histopathologically shows central squamous cell differential with peripheral palisading ameloblastic cells and keratin formation, as seen in our case.
The treatment of ameloblastoma consist of conservative or radical surgery. In radical approach marginal or segmental resection is done with at least safety margin of 1.5-2 cm of normal bone. Radical approach is commonly used for large ameloblastoma or for more aggressive variants whereas, enucleation or enucleation with bone curretage is the common conservative approach used particularly for unicystic type.10 Our case was treated with enucleation of the lesion as a conservative surgery with curettage upto 5mm of bone removal including surrounding healthy bone along with application of Carnoy's solution.
Ameloblastoma has potential for local invasion and has high tendency of recurrence. The recurrence rate varies from the type of treatment performed. Recurrence rate is lesser (13%-15%) for surgical resection while for curettage it is found to be high (90%-100%).4,5 The conventional ameloblastoma has a high recurrence rate compared to unicystic ameloblastoma due to the presence of fibrous connective tissue capsule. Recurrence of the lesion is due to the infiltrative property of the tumor into the cancellous bone. Thus regular follow up is utmost mandatory to evaluate the recurrences in future. We have follow-up the case for more than 2 years with no sign of recurrence, and bone formation in the area of the lesion showing healing.
CONCLUSION:
Though ameloblastoma is the common tumor of the jaw, acanthomatous type of ameloblastoma is very rare. Very few case of acanthomatous ameloblastoma is reported in the literature occurring in elderly aged patient in anterior region of the mandible crossing midline. Also, ameloblastoma has high recurrence rate, so long term follow up is mandatory at regular intervals to rule out recurrence after surgery.
REFERENCES:
- Acanthomatous ameloblastoma of mandible crossing the midline: A rare case report. Ann Afr Med [serial online]. 2015;14:65-8. [cited 2022 Jan 30]
- [CrossRef] [PubMed] [Google Scholar]
- Histological Typing of Odontogenic Tumours. In: WHO International Histological Classification of Tumours (2nd). Berlin: Springer-Verlag; 1992. p. :11-14.
- [CrossRef] [Google Scholar]
- Identification of recurrent SMO and BRAF mutations in ameloblastomas. Nat Genet.. 2014;46(7):722-5.
- [CrossRef] [PubMed] [Google Scholar]
- Update from the 4th Edition of the World Health Organization Classification of Head and Neck Tumours: Odontogenic and Maxillofacial Bone Tumors. Head Neck Pathol.. 2017;11(1):68-77.
- [CrossRef] [PubMed] [Google Scholar]
- Acanthomatous ameloblastoma in anterior mandibular region of a young patient: A rare case report. Ann Afr Med.. 2017;16(2):85-89.
- [CrossRef] [PubMed] [Google Scholar]
- Mandibular ameloblastoma: analysis of surgical treatment carried out in 60 patients between 1977 and 1998. J Craniofac Surg.. 2002;13(3):395-400.
- [CrossRef] [PubMed] [Google Scholar]
- textbook of oral medicine and radiology (2nd). Hyderabad: Paras publisher; p. :161-771.
- Ameloblastomas: current aspects of the new WHO classification in an analysis of 136 cases. Surg Exp Pathol. 2019;2:17.
- [CrossRef] [Google Scholar]
- Recurrent Ameloblastoma: A Surgical Challenge. Case Rep Dent. 2018;2018:8271205.
- [CrossRef] [PubMed] [Google Scholar]
- Recurrence of Plexiform Ameloblastoma as Acanthomatous Ameloblastoma: A Rare Case Report. Contemp Clin Dent. 2019;10(1):178-181.
- [CrossRef] [PubMed] [Google Scholar]







