Translate this page into:
A SPECTRA OF FACIAL AND AURICULAR ANOMALY: BRACHIAL ARCH SYNDROME
Corresponding Author : Dr. Pratiksha Hada
This article was originally published by Indira Gandhi Institute of Medical Science and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Hemifacial microsomia (HFM) is a congenital facial deformity involving the structures derived from first and second pharyngeal arches like temporomandibular joint, mandibular ramus and body, muscles of mastication, ear and sometimes facial nerve. HFM is the second most common developmental craniofacial anomaly after cleft lip and palate, which usually occurs unilaterally, but also may occur bilaterally. In the present article, we have reported a case of HFM in an 18 year old female with unilateral facial hypoplasia and deformed ear.
Keywords
Condylar hypoplasia
hemifacial microsomia
microtia
unilateral hypoplasia
INTRODUCTION:
Hemifacial microsomia (HFM) is a condition characterized by underdevelopment of the first and second branchial arch structures. Hemifacial microsomia (HFM) was first used by Gorlin to refer to patients with unilateral microdontia, macrostomia, and failure of formation of the mandibular ramus and condyle.1 It is the second most common craniofacial malformation after cleft lip and palate. Goldenhar syndrome is considered a variant of this condition that additionally includes epibulbar dermoids and vertebral anomalies. The reported incidence cases of HFM are about 1 in 5600 live births. During the development of the jaw, the neural crest cells migrate to the first pharyngeal arch from the posterior mesencephalic fold and from the first rhombomeres, which gives rise to the skeletal maxillo-mandibular component.2 Damage or disruption of these neural crest cells result in HFM and some related syndromes.
CASE REPORT:
An 18yrs old female patient reported to the department of oral medicine and radiology with a chief complaint of difficulty in mouth opening since childhood. Patient's mother gave no history of forceps delivery or any trauma. On general examination, patient was moderately built and well nourished, cooperative, well oriented to time, place and person, with normal gait and all the vitals were within normal range. Family history was non-contributory.
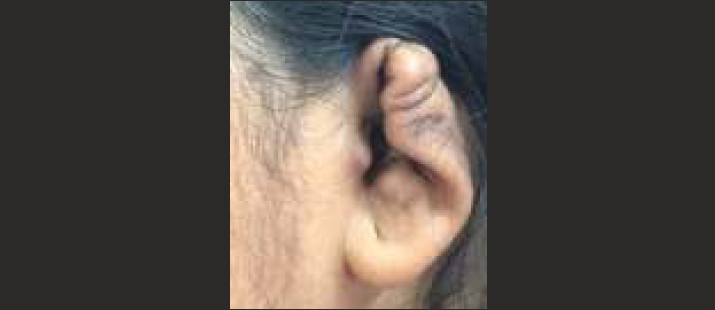
On detailed extraoral examination- there is evident facial asymmetry due to mandibular hypolplasia, deviated chin with fullness of face on left side (figure 1a), as well as malformed ear on same side (figure 1b). The eye, ala of nose and corner of mouth is placed at a higher level on right side. TMJ movements are palpable on right side while lateral excursion movements were restricted.
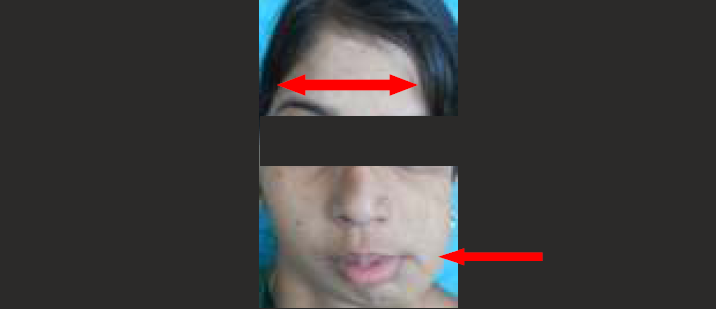
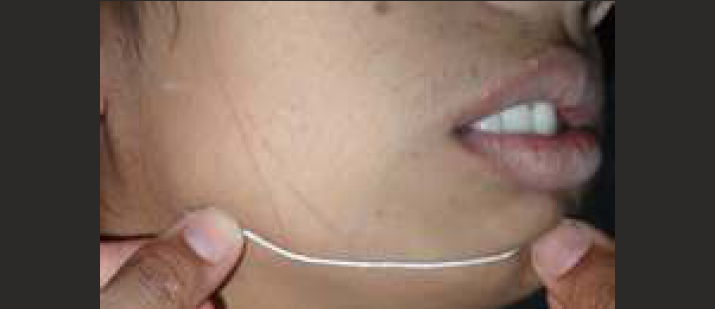
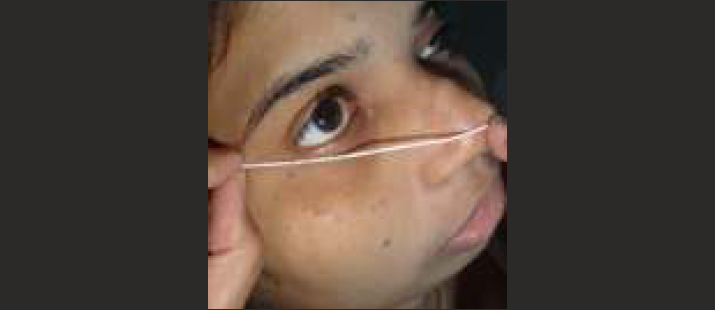
Mandible is deviated on left side during mouth opening along with shifting of midline, distance form chin to angle of mandible is more on right side (90mm) (figure 2) as compared to left side (75mm) (figure 3) similarly distance form tip of nose to outer canthus of eye is more on right side (74mm) (figure 4) as compared to left side (54mm) (figure 5). On palpation tenderness was absent on preauricular region bilaterally, muscles of mastication were also non tender.

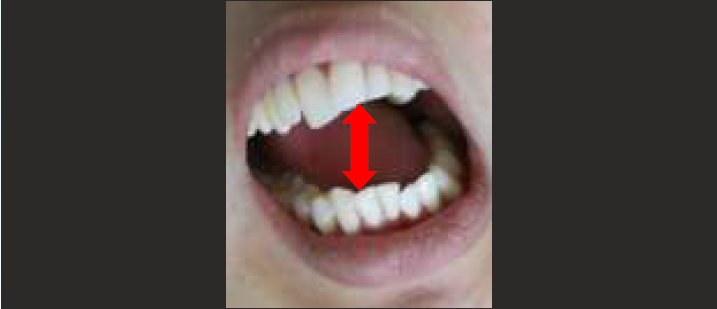
Intraoral examination revealed midline deviation, mesial tilt in vertical axis (figure 6), crowding in upper and lower anteriors and angles class I molar relation on right side and angles class II molar relation on left side. (figure 7, 8)


On the basis of history and clinical examination, a provisional diagnosis of Unilateral anklylosis of left temporomandibular joint was given. The differential diagnosis considered were hemifacial microsomia, hemifacial atrophy and condylar hypoplasia.
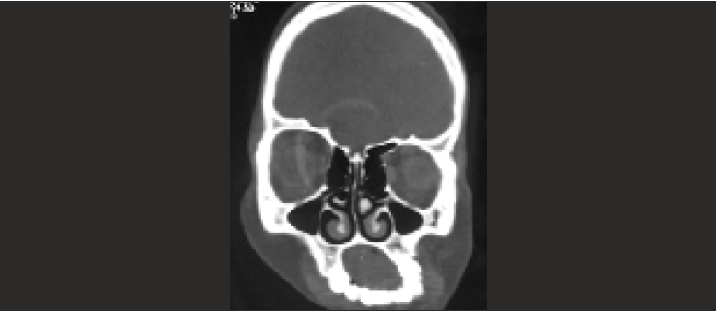
The patient was subjected to panoramic radiograph (OPG) and computed tomography (CT scan). OPG revealed left side mandibular hypoplasia, short ramal height and width, small condylar head, reduced height of mandible, reduced depth of sigmoid notch and prominent antegonial notch. (figure 9) CT scan showed reduced height of left orbit and maxillary sinus with deviated mandible, prominent antegonial notch and small mandibular condyle (figure 10, 11). Thus final diagnosis of Hemifacial microsomia involving left side of face was made. Orthognathic surgery for maxillary and mandibular hypoplasia along with orthodontic treatment was proposed.


DISCUSSION:
The facial deformity caused by hemifacial microsomia is a congenital condition in which the lower half of face is unilaterally under-developed and does not catch-up with the normal growth during childhood. Until now the cause of hemifacial microsomia has been uncertain, although it has mainly been considered to be a developmental abnormality.1,3 The condition seems to have a multifactorial origin and is heterogenous in its clinical appearance.
Synonyms for HM include " otomandibular- dysostosis” or first and second brancial arch syndrome". The two most frequently used classifications are the skeletal-auricular-soft tissue (SAT) and the orbital asymmetry-mandibular- hypoplasia-earmalformation-nerve dysfunction-soft tissue (OMENS) deficiency.4
In 48% of the cases, the condition is a part of a larger syndrome such as Goldenhar syndrome.5 In our case, there was evident facial asymmetry due to mandibular hypoplasia on left side and deviated chin with fullness of face on the left side. There was malformed ear on the left side. Intraorally, tooth size discrepancies, tooth agenesis, supernumerary teeth, malocclusion, enamel and dentine malformations, delayed tooth development and eruption may be present. In this case there was crowding in upper and lower anteriors, class I molar relation on right side and class II molar relation on left side.
Radiographically, OPG and CT scan reveals aplasia or hypoplasia of the mandibular body, ramus and condyle and hypoplastic maxillary and zygomatic bones. In the case reported here, OPG revealed left side mandibular hypoplasia, short ramal height and width, small condylar head and prominent antegonial notch. CT scan revealed reduced height of left orbit and maxillary sinus. Based upon the clinical and radiolographic findings, a final diagnosis of HFM was made. The differential diagnosis of HMF include Pierre Robin Syndrome, Treacher Collin Syndrome and Parry Romberg Syndrome.
Management of HFM is a multidisciplinary approach, with the goal to improve facial symmetry and functioning.6 Considering the age and growth of the individual, the treatment can be broken down into various age segments.7 In our case the age of the patient was 18years, orthognathic surgery along with orthodontic treatment was proposed.
CONCLUSION:
The first step in treating the patients with HFM, is an accurate diagnosis. Many of the craniofacial anomalies can be misdiagnosed, although the treatment of some of these anomalies is like HFM.2,8 Decision making for treatment planning of patients with HFM, is highly dependent on the severity of the deformity and patient's age.9 In mild grades of the anomaly, functional therapy can improve facial and occlusal symmetry in young ones, but in more severe grades, imposition of orthopedic treatment, may be undesirable and waste of time. Early surgical interventions to encourage the growth in the affected condyle may be helpful in severe cases, however, consultation with the surgeon is advised to determine the outcome of the treatment.5,10
REFERENCES:
- Oculoauriculovertebral anomaly: variability and causal heterogeneity. Am J Med Genet Suppl. 1988;4:41-53.
- [CrossRef] [PubMed] [Google Scholar]
- Genetic aspects of the BOR syndrome brachial fistulas, ear pits, hearing loss, and renal anomalies. Am J Med Genet. 1978;2:241-52.
- [CrossRef] [PubMed] [Google Scholar]
- Goldenhar syndrome occurring in one of triplet infants derived from in vitro fertilization with possible monozygotic twinning. Fertil Embryo Transfer. 1985;2:278-32.
- [CrossRef] [PubMed] [Google Scholar]
- Is hemifacial microsomia linked to multiple maternities? Br J Plast Surg. 2002;55(6):474-8. [PubMed: 12479420]
- [CrossRef] [PubMed] [Google Scholar]
- Hemifacial microsomia?A case report and review of literature. Int J Adv Health Sci. 2014;1:9-12.
- [Google Scholar]
- Hemifacial microsomia: A case report. J Indian Soc Pedod Prev Dent. 2008;26(Suppl 1):S34-40.
- [CrossRef] [PubMed] [Google Scholar]
- Craniofacial microsomia: A rare case report. J Oral Maxillofac Radiol. 2013;1:70-4.
- [CrossRef] [Google Scholar]
- Hemifacial microsomia: A rare case report. J Indian Acad Oral Med Radiol. 2015;27:603-7.
- [CrossRef] [Google Scholar]







