A RARE CASE OF BILATERAL OSTEOMA OF THE MANDIBLE
Corresponding Author : Dr. Palak Chaudhary
This article was originally published by Indira Gandhi Institute of Medical Science and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Facial osteomas are a rare occurrence, with only a few cases recorded in the literature. Osteomas are well-differentiated developed bone neoplasms that are generally asymptomatic. It is a benign, slow-growing osteogenic tumour that usually arises from craniofacial bones such the sinus, temporal, or jaw bones, but rarely the mandible. Osteoma is a type of bone that is compact or cancellous and can be peripheral, central, or extraskeletal. Peripheral osteoma is a unilateral, pedunculated mushroom-like mass that originates from the periosteum. In computed tomography, solitary peripheral osteomas are identified by a well-defined, rounded, or oval radiopaque mass. Here we present a rare case of bilateral osteoma of the mandible.
Keywords
Benign neoplasm
cone beam computed tomography
mandible
osteoma.
INTRODUCTION:
Jaffe originally identified osteoid osteoma (OO) in 1935 as a benign osteoblastic tumour with a central core of vascular osteoid tissue and specific histo1ogic characteristics1,2. This lesion's specific nature has yet to be determined. Some authors believe it is a real neoplasm, while others believe it is the result of trauma or an inflammatory process3. The development of compact or cancellous bone characterizes peripheral osteomas of the face bones, which are benign osteogenic tumors. They come from the cranio-maxillofacial area, which includes the temporal bones, sinuses, maxilla, and mandible. They are most common between the second and fifth decades, but they can occur at any age. It accounts for around 10% of all benign bone tumours and is more prevalent in males4. It primarily affects teens and young adults, with a preference for the long bones of the femur and tibia, as well as the vertebra, but it has been seen in a variety of places. There are three subtypes of osteomas are seen, peripheral (parosteal, periosteal, or exophytic), central (endosteal), and extraskeletal (osseous choristoma osteoma). An osteoid osteoma is often monofocal and unilocular. The central type arises from the endosteum, the peripheral osteomas from the periosteum while the extraskeletal soft tissue osteomas often develop within the muscles. It may be multifocal, meaning there are several tumours in a single bone, in exceedingly rare cases. Its incidence in the craniofacial bones has been reported in only a few cases5. The current report describes a very unusual instance of multifocal osteoid osteoma in the jaw that presented bilaterally, with extensive clinical and radiological data.
CASE REPORT:
A 34 year old male patient reported to the department with a chief complaint of pain and swelling in the right and left angle of mandible since one month. The pain was mild and intermittent in nature, increased especially at night, relieved by analgesics, also the pain on left side of jaw increased particularly on touching. The swelling in the right angle of mandible was slow growing, firm to hard in consistency, tender, and no discharge, but the swelling on left side had any such clinical symptoms. There was no prior history of facial trauma and his past medical and dental history were unremarkable. His vital signs were within normal limits. On extraoral examination, the swelling on the right side was well circumscribed, localised, bony hard, measuring about 2 cm on the lower border of the mandible. It was immobile and Fixed to the underlying bone. The skin over the swelling was pinchable and there were no color changes. There was no paresthesia or anesthesia of the face. There was no palpable regional lymphnodes. Intra oral examination was normal.
The patient was advised complete blood picture with SGOT and SGPT. All the values were in normal range. Then we took a CBCT scan. A cone beam computed tomography scan revealed with increased bone resolution and greater overview demonstrated a large, pedunculated and lobulated mass attached to the buccal surface of the right angle of mandible. Also a similar bony growth was seen on the lingual side of left angle. (Fig. 1 &2)
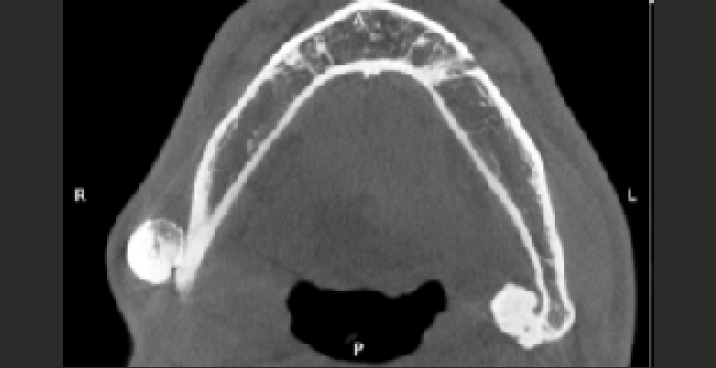
- Axial CBCT Image

- 3D CBCT Image
These clinical and radiographic features were suggestive of provisional diagnosis as peripheral osteoma. The patient was advised for surgical removal of the osteoma bilaterally. The bony lesion was surgically removed with acceptable safety margins and then referred for histological analysis. The histological sample indicated dense compact bone at the periphery with negligible fibrous connective tissue stroma. There were osteoid cells present. As a result, a final diagnosis of mandibular peripheral osteoma was considered.
DISCUSSION:
Due to the small size and self-limiting character of osteoid osteoma, it is referred to as "sui genris." It's a benign bone tumour that accounts for 3% of all primary bone tumours and 10% of all benign bone tumours. Long bones account for around 80% of osteoid ostema. The most common places are the femur, tibia, and vertebrae, with less than 1% of cases occurring in the jaws6, with the lingual surface and lower border of the mandible's body being the most prevalent.
The preceding information about location corresponded to our situation. Only 28 patients with multifocal osteoid osteoma were discovered by Kyriakos et al., with long bones being the most common site of involvement and no jawbone involvement7. A search of the English literature revealed 21 occurrences of osteoid ostemas in the jaws, with five (23.8%) occurring in the maxilla and 16 (76.2%) occurring in the mandible8. Similarly, this case is one of the few reported cases of bilateral osteoid osteoma of the jaw, explaining its rarity.
Peripheral osteoma has an etiopathogenesis that is unknown. Possible etiologic variables include neoplastic and reactive origins, as well as the result of an atypical healing process. However, because there was no history of prior trauma or illness in the case presented in this paper, we have no information about the likely cause. It is more common in boys than females, with a 2:1 ratio, and affects people in their second and third decades of life9. These conclusions were in line with what we had found in our investigation.
Pain is the most commonly reported symptom of osteoid osteoma, which can be constant or intermittent. The pain is usually dull and uninteresting, and it gets worse at night. Golding10 concluded that the lesion's prominent vascular features were to blame for both the pain and the osseous reaction. The strange pain observed in osteoid osteoma, according to Jaffe, is due to the lesion's arteriolar blood supply. Peripheral osteoma manifests clinically as a unilateral, well-circumscribed lump ranging in size from 10 to 40 mm in diameter. Swelling, facial asymmetry, and functional impairment may occur depending on the location and extent of the lesion11. In most cases, the swelling is painless. In our case, the lesion had grown to a great size, causing facial asymmetry as well as other clinical indications.
The appearance of osteoid osteoma on radiographs aids in diagnosis. The nidus was mostly radiolucent, according to Jaffe, and was surrounded by a reactive radiopacity that extended for a variable distance from the nidus. The radiopaque nidus was more common in the less advanced lesion, whereas the radiolucent nidus was more common in the fully mature osteoid osteoma. The calcification of osteoid in the later embryonic stages, according to Prichard and Mckay12, resulted in a central opaque body that varied in density as the calcification advanced. The radiographic image in our case was of a well-defined radiopacity with a radiolucent rim containing a core radiolucent nidus surrounded by a radiolucent border. Differential diagnosis was investigated based on the history and examination, including ossifying fibroma, idiopathic osteosclerosis, cementoblastoma, complex odontoma, osteoblastoma, and osteoid osteoma.
Cone-beam CT imaging, with its higher bone resolution and lower radiation exposure, is an appropriate modality for detecting OO among the existing diagnostic methods. Cone beam CT is particularly useful in identifying OO because the nidus may be tiny and thus undetectable on standard radiographs or CT scans. The cone beam CT in our case revealed a core mineralization that could be distinguished from a peripheral radiolucency, which was bordered by a dense sclerotic bone zone. This matches the radiological description of OO well.
Osteomas are composed of mature lamellar or cancellous bone with extensive fibrofatty marrow between bony trabeculae on histological examination. The standard therapy is a full excision, according to the literature. Following surgery, the spontaneous pain vanishes. The growth of a second lesion or inadequate eradication of the existing lesion are the causes of local recurrence13.
CONCLUSION:
We presented a rare case of bilateral mandibular osteoid osteoma with clinical and radiological features. Because of the tumor's rarity and exceptionality, clinicians must be enigmatically vigilant in order to make a thorough diagnosis and therapy. As a result, case reports and other examples should be addressed in order to raise awareness and strengthen our perception in the relevant subject.
REFERENCES:
- Osteoid osteoma: A benign osteobiastic tumor composed of osteoid and a typica1 bone. Arck Surg. 1935;31:09-28.
- [CrossRef] [Google Scholar]
- Osteoid osteoma: a current review. J. Pediatr. Orthop. 2006;26(965):70.
- [CrossRef] [PubMed] [Google Scholar]
- Osteoid osteoma and osteoblastoma. J Am Acad Orthop Surg. 2011;19(11):678-689.
- [CrossRef] [PubMed] [Google Scholar]
- Intra-articular osteoid osteoma as a differential diagnosis of diffuse mono-articular joint pain. BMC Musculoskelet Disord. 2016;17(1):455.
- [CrossRef] [PubMed] [Google Scholar]
- Osteoblastomatosis of bone. A benign, multifocal osteoblastic lesion, distinct from osteoid osteoma and osteo- blastoma, radiologically simulating a vascular tumor, Skelet. Radiol. 2007;36:237-247.
- [CrossRef] [PubMed] [Google Scholar]
- Unusual osteoid osteoma of the mandible: report of case and review of the literature. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2013;116:134-140.
- [CrossRef] [PubMed] [Google Scholar]
- Natural history of osteoid osteoma with a report of 20 cases. J Bone Joint Surg Br. 1954;36(2):218e29.
- [CrossRef] [PubMed] [Google Scholar]
- "Huge peripheral osteoma of the mandible: a case report and review of the literature," Pathology Research and Practice. 2007;203(3):185-188.
- [CrossRef] [PubMed] [Google Scholar]
- Osteoid osteoma with a multi- centric nidus. Int. Orthop. 1996;20:61-63.
- [CrossRef] [PubMed] [Google Scholar]







