Translate this page into:
A NOVEL PERIODONTAL PLASTIC SURGICAL PROCEDURE FOR PAPILLA RECONSTRUCTION IN ANTERIOR AESTHETIC REGION WITH A VARIANT BEAGLE'S TECHNIQUE- A CASE REPORT
Corresponding author : Dr. Amit Kumar
This article was originally published by Indira Gandhi Institute of Medical Science and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Black triangle, an open interproximal space between maxillary anterior teeth can create aesthetic concern among patients specially while smiling and during speech. There are several risk factors leading to the development of black triangle and the most common among them includes aging, periodontal disease, length of embrasure area, interproximal contact position, triangular- shaped crowns and root angulations. Various techniques like orthodontic correction, prosthetic veneers and various periodontal surgical methods have been used to cover these unesthetic open embrasures. Treating this black triangle can be best done by surgical techniques but it is challenging and very unpredictable. The purpose of this case report is to present a papilla regeneration technique with minimal surgical trauma in the reconstruction of papilla in the maxillary anterior region of a 36-year-old woman who presented with class II interdental papilla loss in 21 and 22 regions according to Nordland and Tarnow's classification. In the present study, a variant technique given by Beagle in 1992 was used to cover this open gingival embrasure. The technique uses a gingival flap from the labial aspect to close the open gingival embrasures thus improving the aesthetic as well as smile of the patient. The results obtained with this technique were satisfactory.
Keywords
Black triangle
gingival flap
reconstruction of papilla
open gingival embrasure
INTRODUCTION:
The interdental papilla fills the embrasure area between two adjacent teeth and is conical in shape for anterior region. It plays an important role in aesthetics and also acts as a biological barrier in protecting underlying periodontal structures.1 Loss of the interdental papilla creates a hollow spaces in between maxillary anterior teeth and is characterized by term "black triangle”. There are several factors which may cause loss of interdental papilla most common cause of this condition in the adult population is the loss of periodontal support due to plaque-associated lesions; other causes include naturally occurring diastemas, divergent roots, a triangular shaped clinical crown, periodontal disease, as a result of periodontal surgical procedures, inappropriate contours of prosthetic restorations, and traumatic oral hygiene procedures.2 Black triangle may cause functional, phonetic, and aesthetic problems. The Depending on size, these black triangles can have an extremely unesthetic appearance that fails to meet the patient's aesthetic demands.
Classification for the loss of interdental papilla was first proposed by Nordland and Tarnow (1998).3 This classification system utilizes few anatomic landmarks which are as follows:
Interdental contact point.
The facial apical extent of the CEJ.
The interproximal coronal extent of the CEJ.
Four categories were identified
Normal:
Interdental papilla fills embrasure space to the apical extent of the interdental contact point/area.
Class I:
The tip of the interdental papilla lies between the interdental contact point and the most coronal extent of the CEJ (Space present but CEJ not visible).
Class II:
The tip of the interdental papilla lies at/or the apical to the interproximal CEJ but coronal to the apical extent of facial CEJ (Interproximal CEJ visible)
Class III:
The tip of the interdental papilla lies level with or apical to the facial CEJ.
Over years, a number of attempts were made to augment the interdental papilla using displaced flaps,4 connective tissue grafts,5-8 and repeated inflammatory stimulation with diverse results.9 This case report is describing a new surgical technique, variant of Beagle's technique,10 to achieve soft tissue augmentation of anterior interproximal space without need of a second surgical site as free soft tissue grafting procedures.
CASE REPORT:
A 30-year-old female patient reported to the Department of Periodontics, Navodaya Dental College Raichur, with the chief complaint of gap between the upper front maxillary teeth. On examination we found that there was a class II papilla recession between 21 and 22. Written and informed consent was obtained from the patient followed by recording detailed medical and dental history. Phase I therapy was done and patient was recalled after 21 days for surgical procedure and strict oral hygiene maintenance was reinforced. Surgical reconstruction of interdental papilla was done using a variant of "Beagle technique” given by Sawai et al.10
AIM OF THE TECHNIQUE
This surgical procedure was done to reconstruct the lost interdental papilla with a slight modification in a beagle's technique in order to prevent the incorporation of fat, from the palatal side, in the undersurface of flap thereby, preventing its vascularization.
SURGICAL PROCEDURE
Intraoral antisepsis was performed by rinsing with 12 % chlorhexidine digluconate for 30 seconds. Adequate local infiltration anesthesia was achieved with 2% lignocaine hydrochloride. A partial thickness flap was raised from the attached gingiva apical to the open embrasure using two vertical and one horizontal incision. The flap was then folded upon itself to obliterate the open embrasure completely. The free end of the flap was sutured with the adjacent gingiva with 4-0 silk suture and a sling suture was placed to pull the papilla coronally and to suspend it between adjacent teeth. Periodontal dressing was applied on labial gingiva and post-operative instructions were given to the patient. Antibiotics and analgesics were administered. The dressing and the sutures were removed after 1 weeks, and oral hygiene instructions were given and healing was found uneventful [Figure 1-9].
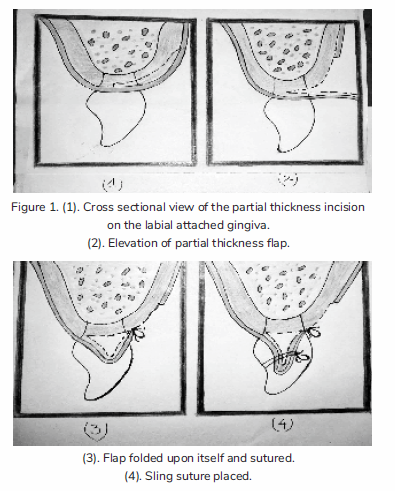

- Preoperative class II papillary recession.

- Incision given with 15 no Bard Parker blade.

- Partial thickness flap elevated.

- Flap reconstructed on desired position.

- Flap pulled coronally with sling suture.

- Periodontal dressing done.

- 1 Week postoperative view.

- 1 Month postoperative view.
DISCUSSION:
Although many techniques have been developed and tried for treating isolated defect in anterior aesthetic region but recreating lost papilla is still a complex phenomenon. In 1985, Shapiro9 proposed a noninvasive approach to recreate papillae destroyed after acute necrotizing ulcerative gingivitis. He induced proliferation of gingival tissue by inflammatory hyperplasia produced after repeated scaling, root planning and curettage. Han and Takie,5 Azzi et al.6-8 etc., proposed different surgical techniques to predictably reconstruct the missing interdental papilla requiring a second surgical site by obtaining connective tissue graft to obliterate the open embrasure space. Beagle (1992)4 presented a technique to reconstruct interdental papilla using the principles of Abram's roll technique and Evian papilla preservation technique which has certain disadvantages i.e., risk of damage to the incisive nerves and vessels and incorporation of fat in the under surface of flap thereby, preventing its vascularization, obtaining a uniform thickness of flap from the palate and retention of periodontal dressing. However, even with these surgical techniques with different flap designs, results are elusive, not predictable and long-term stability are lacking. A major drawback associated with all these techniques is the lack of sufficient blood supply. Any graft placed in this small anatomic area will have to thrive in an unfavorable environment, walled on both side by the non-vascularized tooth surfaces.11 Thus many authors have advocated the use of pedicle/advanced flap for better results than free grafts.10,12
Case selection also plays a pivotal role in the success of the procedure. No improper root angulation or disproportional crown size was present in our case, but interdental contact was not present suggesting of a need for an orthodontic correction along with this procedure, thus making this not a very ideal. But still optimal fill of interdental space was noted.
In this case a small pedicle flap was elevated from labial side and was folded upon itself, sutured with the adjacent gingival and in the end sling suturing was done to suspend it between adjacent teeth. Advantages of this technique include minimal invasiveness, i.e., no second surgical site is required as in case of soft tissue grafts. Furthermore, this procedure is less time-consuming and surgically is a simpler method. To be successful, the surgical procedure must involve the maintenance of the integrity of the interproximal tissue.
CONCLUSION:
The case report shows a novel surgical procedure using pedicle flap folded upon itself to regenerate a lost interdental papilla. The reconstructed papilla in the new position was stable when reviewed at 1 month postoperatively. However, studies with longer study period are required to determine the success rate and the predictability of this procedure. Moreover, of all methods, genuine and stable papillary reconstruction results only when the regeneration of interdental bone occurs. Hence bone grafting along with connective tissue grafting techniques used in conjunction with this surgical technique may increase the chances of obtaining better results so as to aid in restoring gingival aesthetics, thereby, satisfying the patients' aesthetic demands.
REFERENCES:
- Management of inter-dental/inter-implant papilla. J Clin Periodontol. 2005;32:831-9.
- [CrossRef] [PubMed] [Google Scholar]
- Interdental papilla management: A review and classification of the therapeutic approaches. Int J Periodontics Restorative Dent. 2004;24:246-55.
- [CrossRef] [Google Scholar]
- A classification system for loss of papillary height. J Periodontol. 1998;69:1124-6.
- [CrossRef] [PubMed] [Google Scholar]
- Surgical reconstruction of interdental papilla-Case report. Int J Periodontics Restorative Dent. 1992;12:145-51.
- [Google Scholar]
- Progress in gingival papilla reconstruction. Periodontol 2000. 1996;11:65-8.
- [CrossRef] [PubMed] [Google Scholar]
- Surgical reconstruction of the interdental papilla. Int J Periodontics Restorative Dent. 1998;18:467-73.
- [Google Scholar]
- Root coverage and papilla reconstruction in Class IV recession: A case report. Int J Periodontics Restorative Dent. 1999;19:449-55.
- [Google Scholar]
- Root coverage and papilla reconstruction using autogenous osseous and connective tissue grafts. Int J Periodontics Restorative Dent. 2001;21:141-7.
- [Google Scholar]
- Regeneration of interdental papillae using periodic curettage. Int J Periodontics Restorative Dent. 1985;5:26-33.
- [Google Scholar]
- An evaluation of a periodontal plastic surgical procedure for the reconstruction of interdental papillae in maxillary anterior region: A clinical study. J Indian Soc Periodontol. 2012;16:533-8.
- [CrossRef] [PubMed] [Google Scholar]
- Reconstruction of the maxillary midline papilla following a combined orthodontic-periodontic treatment in adult periodontal patients. J Clin Periodontol. 2004;31:79-84.
- [CrossRef] [PubMed] [Google Scholar]







