Translate this page into:
INFLAMMATORY/REACTIVE HYPERPLASIA'S: A REVIEW
Corresponding author : Dr. Smita Lahane
This article was originally published by Indira Gandhi Institute of Medical Science and was migrated to Scientific Scholar after the change of Publisher.
Abstract
The reactive lesions are comparatively common in the oral cavity that dentist face during routine examination because of the frequency with which the tissues are injured. They frequently result from a well-known provocation or injury such as plaque, calculus, or foreign bodies. Diagnosis and development of a treatment plan is difficult if dentists are not aware of the prevalence and clinical symptoms of these lesions. The aim of this article was to review the clinical features of various reactive hyperplastic lesions of the oral cavity. The most commonly found lesions are irritational fibroma, pyogenic granuloma, epulis fissuratum, peripheral giant cell granuloma.
Keywords
Epulis fissuratum
Peripheral giant cell granuloma
pyogenic granuloma
Irritational fibroma.
INTRODUCTION:
Inflammatory hyperplasia is used to describe a large range of usually occurring nodular growths on oral mucosae that histologically represent inflamed fibrous and granulation tissue.1
Reactive hyperplastic lesions are tumor -like hyperplasia which show a response to a low grade irritation or injury such as chewing, food impaction, calculus and overhanging dental restorations. Reactive lesions of the oral cavity are accompanying with injuries of soft tissue and comparatively common oral lesions.2 Kfir et al (1980) have precisely classified reactive hyperplastic lesion into an irritating fibroma, pyogenic granuloma, peripheral giant cell granuloma, and cement-ossifying fibroma.3 These lesions are frequently seen in the gingiva, followed by other areas. Females predilection more than males 4, 5 the age ranged from 1st to 7th decades, with a mean incidence of 2nd -3rd decades.5,6
Classification:
They are classified depending on the location as
-
Occurring only on gingiva
Peripheral ossifying fibroma
Gingival polyp
Gingival enlargement
-
Commonly associated with gingiva
Pyogenic granuloma.
Peripheral gaint cell granuloma.
-
Not occurring on Gingiva
Irritational fibroma
Inflammatory papillary hyperplasia
Pulp polyp
Nodular fasciitis
IRRITATION FIBROMA:
The term "fibroma", which implies a benign neoplastic proliferation of fibrous connective tissue therefore the term "focal fibrous hyperplasia" which recommends a reactive tissue response is more preferable. The lesion appears as a raised mass that is pedunculated or sessile with a smooth surface, and is frequently the same color as that of neighboring mucosa. The distinguish of reactive hyperplasia from true fibromas by the presence of the immunohistologic features (CD34, alpha-SMA, vimentin, Ki-67 and TGF- Alpha) of this irritation fibroma. The frequently involved site is the buccal mucosa along the line of occlusion and sessile lesion on the gingiva, mostly in the interdental papilla of the anterior teeth in adults.7 The size of lesion varied from smaller than 0.5 cm (25.3%), 0.5-1.0 cm (30.14%), and 1.0-1.9 cm (22.58%). The nuchal type fibroma associated with Gardner's syndrome.15 Conventional surgical excision and eradication of irritating factors are the choice of treatment for irritation fibroma with a low recurrence rate.

- irritational fibroma present on the left lateral border of tongue
PYOGENIC GRANULOMA [granuloma pediculatum, benignum, benign vascular tumor, pregnancy tumor, vascular epulis, Crocker and Hartzell's disease.16
Pyogenic granuloma is one of the most communal objects liable for causing soft tissue enlargements. Clinically, the young lesions are highly vascular, red or reddish purple, regularly elevated and ulcerated, and bleed easily, whereas older lesions tend to be extra collagenized and pink in form.7 pyogenic granuloma is a misnomer as the lesion is not associated with pus formation and it is composed of granulation tissue histologically, it show necrotic white material clinically so these lesions refer as pyogenic granuloma10. Almost in one-third of the lesions a history of trauma can be detected pyogenic granuloma may display a rapid growth, but usually reaches its maximum size within weeks or months. The size of the lesion varies from a few millimeters to several centimeters in diameter. In 75% of all cases, the most often affected site is the gingivae followed by the lips, tongue, and buccal mucosa. Maxillary gingivae are more predominant than mandibular gingivae, and anterior areas more frequently involved than posterior area. A female predilection and a propensity to affect children and young adults. Surgical excision is the treatment of choice.10 after surgical excision of gingival lesions, curettage of underlying tissue is suggested. Excision with 2 mm margins at its clinical periphery and to a depth to the periosteum or to the causative agent. Any foreign body, calculus, or defective restoration should be eradiate as part of the excision.18
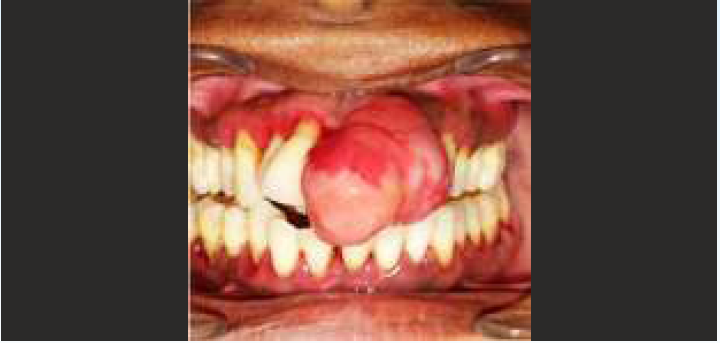
- pyogenic granuloma present in maxillary ant. Region of gingiva in relation with 11,21,22
PERIPHERAL OSSIFYING FIBROMA:
The Peripheral ossifying fibroma is thought to originate from the superficial periodontal ligament and this raised lesion may look smooth and pink or ulcerated and erythematous.7 Lesion regularly less than 2cm in diameter, but up to 8cm have been listed as well. Tooth mobility, tooth migration, and bone destruction have been noted in some cases. This lesion occurs wholly on the gingivae with up to 60% of cases being stated in the anterior areas of the maxilla (incisor cuspid region). Two theories have been suggested to explain the pathogenesis of the lesion: It might originate from a calcified pyogenic granuloma, or it may rise from an overgrowth and proliferation of various components of connective tissue in the periodontium, but the main cause is up till now to be clarify. It is principally a lesion of teenagers and young adults with a peak occurrence being between 10 to19 years. Females are commonly affected than males, primarily during their 2nd decade of life, due to fluctuations of estrogen and progesterone. Treatment usually includes surgical excision, and the lesion should be excised down to the periosteum. The recurrence rate has been assessed to be between 8% and 20%.8

- peripheral ossifying fibroma on maxillary ant.
Region in relation with 21, 22
Image courtesey: Paulo S. G. Henriques, Luciana S. Okajima, Marcelo P. Nunes, Victor A. M. Montalli, "Coverage Root after Removing Peripheral Ossifying Fibroma: 5-Year Follow-Up Case Report", Case Reports in Dentistry, vol. 2016, Article ID 6874235, 6 pages, 2016. https://doi.org/10.1155/2016/6874235
PERIPHERAL GIANT CELL GRANULOMA
[peripheral giant cell tumor, osteoclastoma, reparative giant cell granuloma, giant cell epulis and giant cell hyperplasia of the oral mucosa.
Peripheral gaint cell granuloma is one of the most frequent giant cell lesions of the jaws and initiates from the connective tissue of the periosteum or the periodontal membrane. It is not a true neoplasm but somewhat a benign hyperplastic reactive lesion occurred in response to local irritation such as tooth extraction, poor dental restorations, ill-fitting dentures, plaque, calculus, food impaction, and chronic trauma. Clinically, it demonstrates as a firm, soft, bright nodule or as a sessile or pedunculated mass and with sporadically ulcerated surface. The color of lesion, varies from dark red to purple or blue. It is situated in the interdental papilla, edentulous alveolar margin or at the marginal gingival level.7 The mandible is predominant than the maxilla, it is usually less than 2 cm in diameter, but larger sizes are seen seldom. Progressive growth in some cases causes' bone and root resorption8 giving cup-shaped radiolucency called cupping resorption.

- peripheral giant cell granuloma present on mandibular anterior region of gingiva in relation to 31, 32,33,34,35,
(Abhay K, Rajendra B, Sanjeev O, A Reticent Intraoral Growth - Peripheral Giant Cell Granuloma, Journal of Periodontal Medicine & Clinical Practice, vol-2, issue- 1, jan-April, 2015)
Epulis Fissuratum
[denture induced hyperplasia] Epulis fissuratum is a reactive lesion of the oral cavity commenced by low grade chronic trauma from dentures. The lesion seems as an asymptomatic single fold or multiple folds of hyperplastic tissues in the alveolar vestibule along denture flanges with a smooth surface, soft to firm consistency, and a normal in color. Rarely in the bottom of the folds, severe inflammation or ulceration may be seen. Maxilla affected more than the mandible, entirely on the facial aspect of the alveolar ridges .the size varies from <1 cm to huge lesion. It is manage conservatively or surgically depending on the size of the lesion.8

- epulis fissuratum giving as an exophytic with smooth surface accompanying with an ill-fit mandibular denture.
{Image courtesey: Hamed Mortazavi, Yaser Safi, Maryam Baharvand, Somayeh Rahmani, Soudeh Jafari, "Peripheral Exophytic Oral Lesions: A Clinical Decision Tree", International Journal of Dentistry, vol. 2017, Article ID 9193831, 19 pages, 2017. https://doi.org/10.1155/2017/9193831}
Inflammatory papillary hyperplasia:
Inflammatory papillary hyperplasia (IPH) is a benign lesion of the oral mucosa which is characterized by the growth of one or more nodular lesions, determining about 2mm or less. The lesion almost entirely involves the hard palate. Nevertheless, in rare instances, it also has been seen on the mandible. The lesion is mostly asymptomatic and the color of the mucosa may vary from pink to red.11 these lesions in inflammatory stage look as red, soft masses and convert to pink and firm when they mature to fibrous stage. It can occur at any age .but, most commonly occur in the 3rd to 5th decade of life with a male predilection. In to ill-fitting denture, Candida albicans has an etiologic role. Less extensive lesions are subside by eradicating the denture at night and improving oral hygiene. Patients can also benefit from antifungal agents. Various surgical methods have been recommended for the treatment of this lesion such as excision of partial thickness or full thickness, curettage, cryosurgery and electro surgery.

- Upper edentulous ridge showing papillary nodules at the labial aspect of the ridge.
Image courtesy: Samiha Yousef Sartawi, Shaden Abu-Hammad, Nesreen A. Salim, and Salah Al- Omoush, International Journal of Dentistry Volume 2 0 2 1, Article ID 7338143, 8 pages https://doi.org/10.U55/2021/7338143
Pulp polyp
[chronic hyperplastic pulpitis or proliferative pulpitis or pulpitis aperta] Clinically it seem like as proliferative red mass seen in the occulsal portion of the molars in individuals with higher immunity. It is the protective reaction against the tissue inflammation causing in hyperplastic changes. It is occasionally associated with mild pain along with large carious cavitated lesions and may be related with rare history of bleeding. Histologically it shows abundant granulation tissue with many blood vessels.14 it appears as a smooth, soft to firm, red to pink, pedunculated, or sessile mass conquering the entire carious cavity in the involved tooth similar to an enlarged gingival tissue. The size of the lesion varies from < 1cm in diameter to large masses (about 4cm).8

- Pulp polyp related with carious primary first mandibular molar.
GINGIVAL POLYP
[localized gingival enlargement or epulis]
Gingival Polyp, which are focal fibrous hyperplastic lesion. It purely represent a reactive hyperplasia of fibrous connective tissue in response of trauma or irritation. The prime reason for the incidence of gingival polyp is ascribed to local factors such as caries, overhanging margin, calculus and tooth malposition. It can develop in the proximal tooth cavity near the gum area similar as class II cavity. Rarely, It swollen pale pink gums, enlarge to fill the area in the tooth cavity. It usually occurs in border area cavity of the teeth with adjoining teeth (class II cavity).3 Enlargement of the gum can be abridged by incision, minor surgical procedures, undergone anesthetized conditions. The gold standard for this treatment is surgical excision performed with a scalpel, electrocautery or lasers.16

- gingival polyp present in carious proximal surface of 1st mandibular molar.
| GINGIVAL POLYP | PULP POLYP | |
|---|---|---|
| Origin | Originates from gingiva. | Originates from pulp |
| Spread | Runs towards center | Runs outwards from the center |
| Base | Broad base | Narrow stalk |
| Tooth surface involved | Proximal surface | Occlusal surface |
| Attachment | Can be separated from the tooth | Attached to the tooth |
| Bleeding on probing | Bleeds easily on probing. | May not bleed easily |
| Treatment | Excision / local debridement. | Endodontic / Extraction |
Nodular Fasciitis and Proliferative Myositis
Nodular fasciitis, a non-neoplastic connective tissue proliferation, usually happens on the trunk or extremities of young adults. It appears as a rapidly growing nodule that histologically mimics a malignant mesenchymal neoplasm (sarcoma) but that clinically acts in a benign fashion. It encounter at all ages, with the majority during the 4th and 5th decades. Has no gender predilection. The most communal oral site is the buccal mucosa, maximum have an exophytic pre- sentation, and growth rates are variable. It has specific microscopic features that permit for the diagnosis, and the principal cell type is the myofibroblasts. Proliferative myositis and focal myositis are lesions of skeletal muscle that have analogous clinical features and are differentiated by histopathologic findings. Rare cases seen in the tongue and in other neck and jaw muscles. Proliferative myositis is a reactive fibroblastic lesion that infiltrates around individual muscle fibers. In spite of the terminology, these lesions do not show histologic signs of inflammation.1
GINGIVAL ENLARGEMENT
Inflammatory gingival enlargement:
Inflammatory gingival enlargement occurs in locations of poor oral hygiene where there is accumulation of plaque, supra-gingival calculus formation, impaction of food, or the existence of provoking factors like hormonal changes or other systemic diseases. The clinical diagnosis of is forthright, with tissues displaying a glossy edematous bright red or purplish red color and a tendency to hemorrhage on slight provocation. A fetid odor may outcome from the decomposition of food debris and buildup of bacteria. In long-standing cases of inflammatory enlargement, there may be an accompanying loss of periodontal attachment leading to periodontal disease. Affecting principally the maxillary anterior region may be detected in mouth breathers. Hormonal changes (such as during pregnancy or puberty) may amplify the local immune response to local factors The impaired collagen synthesis accompanying with vitamin C deficiency (scurvy) may also complicate inflammatory gingival enlargement. Amplify the local immune response to local factors and contribute to gingival enlargement. Treatment begins with the establishing of excellent oral hygiene, along with the eradication of all local and/or systemic predisposing factors if possible. This contains a professional debridement (supragingival scaling or subgingival root planing) and prophylaxis and improving of faulty restorations, carious lesions, or food impaction site.1

- inflammatory gingival enlargement present on lower anterior region of gingiva.
CONCLUSION:
The inflammatory and reactive hyperplastic leasions present usually in oral cavity secondary to injury and local factors which can imitator benign and rarely malignant lesions. The complete removal of local irritants with follow-up and maintenance of oral cleanliness helps to prevent the recurrences of such lesions. We included a classification regarding oral peripheral exophytic lesions, divided into lesions occurring only on gingiva, commonly associated with gingiva and not occurring on gingiva. Upon confronting a peripheral exophytic mass in the oral cavity a clinician should have knowledge about the some features such as surface texture, shape, color, and consistency in order to categorize the lesion, and progress along the decision to reach a logistic differential diagnosis.
Declarations:
Conflict of interest:
None
Ethical approval:
None
Funding:
None
REFERENCES:
- Benign lesion of oral cavity J Kerr Ross A, DDS, MSD Joan A. Phelan, DDS, Bucket's oral medicine.
- [Google Scholar]
- Reactive hyperplastic lesions of the oral cavity. Iran J Otorhinolaryngol. 2015;27(79):137-44.
- [PubMed] [PubMed Central] [Google Scholar]
- Reactive hyperplastic lesions of the oral cavity: A ten year observational study on North Indian Population. J Clin Exp Dent. 2012;4(3):e136-40. eCollection 2012 Jul.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Reactive hyperplastic lesions of the oral cavity: A retrospective survey study and literature review. Indian J Dent Res. 2018;29(1):61-66. Review
- [CrossRef] [PubMed] [Google Scholar]
- Incidence of reactive hyperplastic lesions in the oral cavity: a 10 year retrospective study in Santa Catarina, Brazil. Braz J Otorhinolaryngol. 2019;85(4):399-407. Epub 2018 Apr 17
- [CrossRef] [PubMed] [Google Scholar]
- Reactive localised inflammatory hyperplasia of the oral mucosa. East Afr Med J. 2009;86(2):79-82. PubMed PMID: 19894472
- [CrossRef] [PubMed] [Google Scholar]
- Reactive lesions of oral cavity: A survey of 100 cases in Eluru, West Godavari district. Contemp Clin Dent. 2012;3(3):294-7.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Peripheral Exophytic Oral Lesions: A Clinical Decision Tree. 1nternational Journal of Dentistry. ;2017 Article ID 9193831
- [CrossRef] [PubMed] [Google Scholar]
- Pattern of distribution of reactive localised hyperplasia of the oral cavity in patients at a tertiary health institution in Nigeria. Afr Health Sci. 2019;19(1):1687-1694.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- "An extensive denture-induced hyperplasia of maxilla," Annals of Medical and Health Sciences Research. 2013;3(5):7.
- [CrossRef] [PubMed] [Google Scholar]
- "Inflammatory papillary hyperplasia: supraperiosteal excision by the bladeloop technique.," General dentistry. 1998;46(4):390-397.
- [Google Scholar]
- Differential Diagnosis of Oral And Maxillofacial Lesions. (5th). St. Louis, Mo, USA: Mosby; 1997.
- [Google Scholar]
- "Recurrent epulis granulomatosa: a second look," Journal of Advanced Clinical & Research Insights. 2015;2:140-142.
- [CrossRef] [Google Scholar]
- Pulp polyp -A periapical lesion: Radiographic observational study. J Indian Acad Oral Med Radiol. 2015;27:68-71.
- [CrossRef] [Google Scholar]
- Gardner's syndrome associated fibromas. Pathol Int. 2004;54(7):523-526.
- [CrossRef] [PubMed] [Google Scholar]
- Management of gingival polyp in restoration procedure: A case report. Journal of Dentomaxillofacial Science. 2021;6(2):132-135.
- [CrossRef] [Google Scholar]
- "Coverage Root after Removing Peripheral Ossifying Fibroma: 5-Year Follow-Up Case Report" 2016. Case Reports in Dentistry. 2016:6. Article ID 6874235
- [CrossRef] [PubMed] [Google Scholar]
- Oral pyogenic granuloma: Various concepts of etiopathogenesis. J Oral Maxillofac Pathol. 2012;16:79-82.
- [CrossRef] [PubMed] [Google Scholar]
- International Journal of Dentistry. ;2021:8. Article ID 7338143
- [CrossRef]
- A Reticent Intraoral Growth -Peripheral Giant Cell Granuloma. Journal of Periodontal Medicine & Clinical Practice. 2015;2(1)
- [Google Scholar]







